What are noroviruses?
Noroviruses are non-enveloped, RNA viruses that belong to the Caliciviridae family. As the most common cause of acute gastrointestinal infections worldwide and the leading cause of foodborne illness in the United States, norovirus is responsible for approximately 20–21 million and 685 million reported cases each year in the United States and worldwide, respectively (CDC, 2024b). Noroviruses are genetically diverse and can be found in various environments including water, soil, food, and contact surfaces. Among the more than 36 identified strains of norovirus, only a few can infect humans. In addition to the name "norovirus," they also have been known as "Norwalk virus," "Norwalk-like virus" (NLV), and "winter vomiting disease." The World Health Organization (WHO) Foodborne Disease Burden Epidemiology Reference Group (FERG) recently issued a comprehensive report estimating the global burden of foodborne diseases and ranked human norovirus as the number 1 cause of foodborne illness, the number 4 cause of foodborne deaths, and the number 5 cause of foodborne disability-adjusted life years (DALYs)3 (CDC, 2024b). The estimated economic burden of human norovirus is estimated to be $60 billion worldwide due to the healthcare cost and productivity loss.
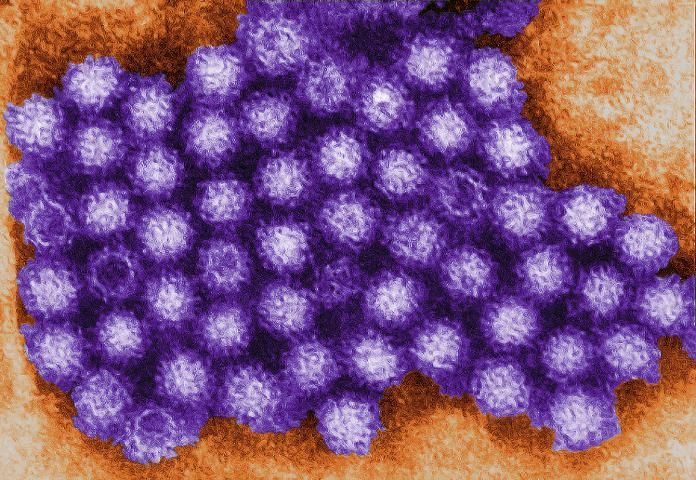
Credit: CDC/Charles D. Humphrey
What causes norovirus-induced foodborne illness?
Transmission mainly occurs via fecal-orally or vomit-orally routes. Norovirus, similar to other viruses, require a living host for replicating. To do so, norovirus particles must enter the host's gastrointestinal tract through the ingestion of contaminated food, water or aerosolized vomit, contact with contaminated objects, or person-to-person contact. As few as 18 norovirus particles can be enough to cause illness in human (CDC, 2014; 2024b). Global surveillance data indicates that approximately 14% of all norovirus outbreaks are primarily foodborne (Verhoef et al., 2015). However, a single outbreak is often characterized by multiple transmission routes because the highly contagious nature of the pathogen allows for rapid secondary person-to-person or environmental transmission.
What are the symptoms associated with noroviruses?
Infection with norovirus causes acute gastroenteritis, which is inflammation of the stomach and intestines. Although symptoms typically begin within 12 hours of ingestion of infectious virus particles, some may manifest as late as 48 hours after exposure. Symptoms may include:
- Nausea
- Vomiting
- Diarrhea
- Stomach cramps
- Headaches
- Fever/chills
- Muscle aches
- Fatigue (a general sense of tiredness)
Symptoms usually resolve without medical intervention and most people with norovirus illness get better within 1 to 3 days. However, it is important to note that even after symptoms end, the infected individuals will continue to shed infectious virus particles in their stool for several weeks.
Who is at risk?
Anyone exposed to contaminated food, water or contact surfaces is at risk for norovirus infection. Even though the illness is usually mild and self-limiting, in case of severe and prolonged infection in immunocompromised individuals, infants, and the elderly, it may lead to hospitalization because of dehydration and loss of electrolytes (Karst, 2010). Due to the environmental stability and highly contagious nature of the human norovirus, individuals in semi-closed communities such as hospitals, day care centers, retirement centers for the elderly, schools, prisons, and cruise ships are at higher risk of large-scale outbreaks (Karst, 2010).
A suitable vaccine for norovirus is not currently available. Development of a norovirus vaccine is challenging because infection with this virus does not bring about the typical protective immune responses normally produced by the human body. Because norovirus is genetically diverse and constantly undergoes genetic mutation, once a vaccine is developed it will likely require continual reformulation like the way the flu vaccine is reformulated each flu season. Several groups are working on the development of a norovirus vaccine, and it appears these vaccines are able to elicit antibody responses against noroviruses (Atmar et al., 2015; Ramani et al., 2017). A recent study shows promising result on norovirus vaccine tested in clinical trials and, as of this report, are being taken forward in clinical development (Leroux-Roels et al., 2018).
Common Settings of Norovirus Outbreaks
Healthcare facilities: The most common reported settings in the US and other industrialized countries where norovirus outbreaks have occurred are healthcare facilities, including long-term care facilities and hospitals. More than 62% of norovirus outbreaks reported in the US occur in health care facilities (CDC, 2024a) and 70% are caused by infected food workers (CDC, 2014).
Restaurants and catered events: Epidemiological studies have shown that food workers have implicated most foodborne norovirus outbreaks in the US. Foods that are commonly involved in norovirus outbreaks include leafy greens, fresh fruits, and oysters.
Schools and child care centers: Norovirus outbreaks also frequently occur in schools, child care centers, colleges, and universities. Several outbreaks have even led to campus closures (CDC, 2024b).
Cruise ships: Cruise ships account for a small percentage (1%) of reported norovirus outbreaks. Norovirus is most often the most frequent cause (over 90%) of outbreaks of diarrheal disease on cruise ships (over 90%). Outbreaks generally originate in the passenger population and then spread to the crew, which can increase the likelihood of infection of passengers on subsequent sailing.
What foods have been commonly associated with norovirus?
According to the surveillance of foodborne outbreaks in the US, the CDC reported that norovirus, among the cases with a single confirmed etiology, was the principle cause of outbreaks during 2009–2015 (Dewey-Mattia et al., 2018). Most foodborne outbreaks of norovirus occur in restaurant or catering settings and are the result of contamination that takes place during food preparation. Food service workers may contaminate food by neglecting proper hand-washing, handling ready-to-eat (RTE) foods with bare hands, and working while ill (Hall et al., 2014). Examples of RTE foods include sandwiches, salads, and baked goods. Liquid items that do not require further processing such as cake icing or salad dressing often cause widespread outbreaks because the virus becomes evenly distributed throughout the product.
Additionally, filter-feeding shellfish such as oysters and clams present an elevated hazard because they ingest norovirus if it is present in surrounding water and concentrate it to much higher levels. Although norovirus cannot reproduce in marine water, it can survive for extended period of times in the environment once introduced. Sources of norovirus contamination to marine water can include faulty wastewater treatment facilities, storm water runoff, dumping of raw sewage, and overboard discharge of vomit near shellfish harvest beds (DOHWa, 2013). Acute gastroenteritis outbreaks associated with contaminated shellfish have been reported all over the world. In 2013, norovirus was detected in 9% of oysters collected on the French market over a period of 16 months (Schaeffer et al., 2013). In addition, a total of 176 cases of gastrointestinal illness linked to oyster consumption were reported in three Canadian provinces: British Columbia (137), Alberta (14), and Ontario (25), where individuals became sick between mid-March and mid-April 2018 (Govt. of Canada, 2018).
How do noroviruses spread?
Infection and spread may occur by
- Eating or drinking contaminated foods (such as oysters, berries, cilantro, etc.), water or beverages
- Touching surfaces or objects contaminated with norovirus, and then using unsanitary/bare hands in food preparation
- Direct contact with a person who is infected (for example, when caring for someone who is ill, or sharing the food or utensils)
- Improper personal hygiene after using the restroom (i.e., not washing hands with soap and water) and then touching surfaces or food to be used by others
- Unaffected persons ingesting virus particles aerosolized by an infected person vomiting nearby
What sanitation methods are used to prevent infection?
Prevention of foodborne norovirus infection is based on the provision of safe food and water. Noroviruses are relatively resistant to environmental challenge: they are able to survive freezing temperatures as well as temperatures as high as 140°F (60°C) and have even been associated with illness from steamed shellfish. Noroviruses can survive in up to 10 ppm chlorine solution, which is well in excess of levels routinely present in municipal water (~1 ppm). Despite these resistances, relatively simple measures such as correct handling of cold foods, frequent hand washing, and disinfection of potentially contaminated surfaces may substantially reduce foodborne transmission of noroviruses. While such practices are easily achievable, they are ineffective if not enforced.
The following are examples provided by the CDC on how to prevent infection caused by norovirus:
- Since norovirus is found in the feces and fluids of infected individuals, it is imperative that proper hand washing techniques (see below) be followed after using the restroom and before preparing, handling, or consuming foods.
- Infected or symptomatic persons should not prepare or handle food.
- Food, clothing (see below), or other surfaces potentially exposed to noroviruses should be immediately disinfected.
- Food should be discarded or thoroughly heated at temperatures greater than 140°F to ensure inactivation of the virus.
- Surfaces should be cleaned with a chlorine bleach solution with a concentration of approximately 1000 to 5000 ppm (5 to 25 tablespoons of household bleach [5% to 8%] per gallon of water) followed by a thorough water rinse to remove any residual bleach.
- Raw fruits and vegetables should be properly washed before consumption or use in food preparation.
- Raw sewage, including soiled diapers, should be properly and sanitarily disposed off.
- Shellfish should be properly cooked prior to consumption. According to the National Fisheries Institute (NFI) and the Food and Drug Administration (FDA), to prevent norovirus infection shucked shellfish (clams, mussels, and oysters without shells) should be boiled for three minutes, fried in oil at 375°F (191°C) for 10 minutes, or baked at 450°F (232°C) for 10 minutes.
- Many local and state health departments require that food handlers with gastroenteritis not work until two or three days after their symptoms improve—be aware of your local regulations.
- Businesses should keep sick children or children wearing diapers away from food preparation areas.
- Wash hands, utensils, and food contact surfaces (FCSs) with hot soapy water after they contact raw meat or seafood, before food preparation, and after using the bathroom.
- Immediately remove and wash clothes or linens that may be contaminated with vomit or stool. People should wear gloves and handle soiled items carefully without agitating them. They should wash them with detergent at the maximum available cycle length and then machine dry the items.
How can food handlers prevent the spread of norovirus infection?
The number one method of avoiding contamination of food with viral, bacterial, and parasitic disease is for all food handlers to regularly and properly wash their hands. While regular hand washing is recommended, some events that should always be followed by thorough washing with soap and warm water for 20 seconds include
- Before handling, preparing, or serving food.
- Before handling clean utensils or dishware.
- After using the restroom.
- After touching your face, cuts, or sores.
- After smoking, eating, or drinking.
- After handling raw meat—especially poultry.
- After touching unclean equipment, working surfaces, soiled clothing, soiled wiping cloths, etc.
- After collecting and taking out the garbage.
- Before and after assisting someone with diarrhea, after cleaning the bathroom, and after changing diapers.
What is the proper procedure for hand washing?
- Wet your hands with warm water.
- Apply soap and wash your hands for 20 seconds.
- Pay attention to hard-to-reach areas like knuckle creases, between fingers and under finger nails.
- Include the forearm past the wrist as you wash.
3. Rinse and then dry with a single-use paper towel.
Some other hygienic tips are
- Do not share food, drinks, spoons, or straws.
- If you have a child in day-care who has diarrhea, inform the day-care providers; they can make sure germs are not spread to other children.
- Do not let anyone who has diarrhea use a pool or swim in a pond while they are sick.
References
Atmar, R. L., D. I. Bernstein, G. M. Lyon, J. J. Treanor, M. S. Al-Ibrahim, D. Y. Graham, J. Vinje, X. Jiang, N. Gergoricus, R. W. Frenck, C. L. Moe, W. H. Chen, J. Ferreria, J. Barrett, A. R. Opekun, M. K. Estes, A Borkowski, F. Baehnet, R. Goodwin, A. Edmonds, P. M. Mendelman. 2015. "Serological Correlates of protection against a GII.4 Norovirus." Clin Vaccine Immunol 22(8):923–929.
Centers for Disease Control and Prevention (CDC). 2014. "Preventing Norovirus Outbreaks: Food service has a key role." CDC Vital Signs. Available at: http://www.cdc.gov/vitalsigns/pdf/2014-06-vitalsigns.pdf. Accessed December 5, 2024.
Centers for Disease Control and Prevention (CDC). 2024a. Norovirus: Facts for Food Handlers. Available at: https://www.cdc.gov/norovirus/media/pdfs/2024/04/norovirus-illness_facts-for-food-handlers_3.20.24.pdf. Accessed December 5, 2024.
Centers for Disease Control and Prevention (CDC). 2024b. Norovirus Facts and Stats.
Centers for Disease Control and Prevention (CDC). 2024c. NoroSTAT data table. Available at: https://www.cdc.gov/norovirus/php/reporting/norostat-data.html. Accessed December 5, 2024.
Centers for Disease Control and Prevention (CDC). 2024d. Outbreaks on Cruise Ships in VSP's Jurisdiction. Available at: https://www.cdc.gov/vessel-sanitation/cruise-ship-outbreaks/?CDC_AAref_Val=https://www.cdc.gov/nceh/vsp/surv/gilist.htm. Accessed December 5, 2024.
Dewey-Mattia D, K. Manikonda, A. J. Hall, M. E. Wise, and S. J. Crowe. Surveillance for Foodborne Disease Outbreaks—United States, 2009–2015. 2018. MMWR CDC Surveill Summ 67(10):1–11. Available at: https://www.cdc.gov/mmwr/volumes/67/ss/ss6710a1.htm. Accessed December 5, 2024.
Government of Canada. 2018. Public Health Notice-Outbreak of norovirus and gastrointestinal illnesses linked to raw oysters Available at: https://www.canada.ca/en/public-health/services/public-health-notices/2018/outbreak-norovirus-infections-linked-raw-oysters.html. Accessed December 5, 2024.
Hall, A. J., M. E. Wikswo, K. Pringle, H. Gould, and U. D. Parashar. 2014. "Vital Signs: Foodborne Norovirus Outbreak—United States, 2009–2012." Morbidity and Mortality Weekly Report (MMWR).63 (22):491–495. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6322a3.htm?s_cid=mm6322a3_w. Accessed December 5, 2024.
Karst, S. M. 2010. "Pathogenesis of noroviruses, emerging RNA viruses." Viruses 2(3):748–781.
Leroux-Roels G, J. P. Cramer, P. M. Mendelman, J. Sherwood, R. Clemens, A. Aerssens, I. De Coster, A. Borkowski, F. Baehner, and P. Van Damme. 2018. Safety and immunogenicity of different formulations of norovirus vaccine candidate in healthy adults: a randomized, controlled, double-blind clinical trial. J Infect Dis 217(4):597–607.
Ramani, S. F.H. Neill, J. Ferreria, J. J. Treanor, S. E. Frey, D. K. Topham, R. R. Goodwin, A. Borkowski, F. Baehner, P M. Mendelman, M. K. Estes, R. L. Atmar. 2017. "B-cell responses to intramuscular administration of a bivalent virus-like particle human norovirus vaccine." Clin Vaccine Immunol 24(5):1–13.
Schaeffer, J., J. Le Saux, M. Lora, R. Atmar, and F. Le Guyader. 2013. "Norovirus contamination on French marketed oysters." Intl J Food Microbiol 166(2):244–248.
Verhoef, L., J. Hewitt, L. Barclay, S. Ahmed, R. Lake, A. Hall, B. Lopman, A. Kroneman, H. Vennema, J. Vinjé, K. Koopmans. 2015. "Norovirus Genotype Profiles Associated with Foodborne Transmission, 1999–2012." Emerg Infect Dis 21(4):592–599.
Washington State Department of Health (DOHWa). 2013. "Norovirus in Shellfish." Available at: https://doh.wa.gov/community-and-environment/shellfish/recreational-shellfish/illnesses/norovirus. Accessed December 5, 2024.