The Centers for Disease Control and Prevention (CDC) estimates that 48 million Americans acquire foodborne illness every year, 128,000 are hospitalized, and 3,000 die (CDC 2011). In 2013, 12% of all foodborne illnesses with a single reported setting (86 outbreaks and 1,078 reported instances of illness) were attributed to food preparation occurring in private homes. Many cases of foodborne illness are not reported, and of those that are, the causative agent is not investigated or identified. In 2013, the top five identified bacterial and viral foodborne illness agents attributed to home food preparation were Salmonella; norovirus; shiga-toxin-producing Escherichia coli (e.g., serovars O104, O111, O157:H7 and others); Clostridium perfringens; and Campylobacter (Scallan et al. 2011).
Household Risks and How They Occur
Salmonella
Food poisoning from Salmonella infections can cause serious illness and even death; symptoms include acute diarrhea, vomiting, dehydration, septicemia, or bacteremia (i.e., bacteria in bloodstream) (Bell and Kyriakides 2009a). Possible secondary illnesses associated with this infection are reactive arthritis, meningitis, and urinary-tract infections, etc. In home-kitchen settings, Salmonella is often linked to egg and egg-based products like homemade mayonnaise in which the choice of acidulant (acetic acid vs. citric acid) and other factors influence the survival of Salmonella introduced through contamination of raw eggs (Radford et al. 1993). Chicken and other poultry, produce, fruits, chocolate, and nuts have also been implicated as vehicles of Salmonella transmission. These food sources may become contaminated with Salmonella by contact with fecal matter (either directly or through cross-contamination), inadequate cooking techniques, and cross-contamination due to poor personal hygiene or improperly cleaned equipment.
Norovirus
Noroviruses are responsible for 20 million reported cases of acute gastroenteritis, or stomach flu, each year (CDC 2024). Symptoms typically begin within 12 hours of ingestion of contaminated food and may include nausea, vomiting, diarrhea, abdominal cramps, headaches, fever/chills, and muscle aches. Norovirus is highly contagious and contact with as few as 100 virus particles is sufficient to cause illness. Foodborne norovirus transmission can occur anywhere people consume food prepared by others. In home-kitchen settings, food can be easily contaminated through handling by infected persons, contact with infectious stool or vomit on kitchen surfaces, or contact with aerosolized vomitus droplets from an infected person (CDC 2024).
Shiga-Toxin-Producing Escherichia coli (STEC)
Shiga-toxin-producing Escherichia coli (STEC) bacteria, such as E. coli O157:H7, can cause severe abdominal cramping, bloody diarrhea, and vomiting (Bell and Kyriakides 2009b). STEC infections can lead to hemolytic uremic syndrome (HUS), which is potentially fatal, especially in young children. E. coli O157:H7 infections occur when people consume contaminated food or water products, including undercooked meat, unpasteurized milk products, and leafy green vegetables. Between 2003 and 2012, ground beef and leafy greens were implicated as the source of more than 25% of all reported E. coli outbreaks in the United States (Heiman et al. 2015). In home-kitchen settings, washing contaminated ready-to-eat leafy greens in tap water may have the unintended effect of cross-contaminating previously uncontaminated portions, thus increasing the potential for STEC infection (Jensen et al. 2015).
Clostridium perfringens
As the second-most common bacterial agent of foodborne illness in the United States, Clostridium perfringens affects nearly one million individuals each year (Grass et al. 2013). Only a fraction of these cases are actually reported due to the mild, self-limiting nature of resultant symptoms. Generally, individuals experience abdominal pain, stomach cramps, and diarrhea within 6–24 hours after consuming contaminated food. High-protein foods of animal origin, including meat and meat products, stews, broth, soups, gravies, milk, etc., are commonly implicated as sources of C. perfringens infection. Because the bacteria is naturally present in the normal intestinal flora of animals, proper cooking of food to an internal temperature of 165°F or higher for at least 15 seconds is necessary to inactivate the bacteria. Additionally, cooked food should be kept hot at 140°F before serving or rapidly cooled to 41°F for storage (FDA 2013).
Campylobacter
Campylobacter is the primary cause of a type of foodborne gastroenteritis known as campylobacteriosis. Resulting symptoms appear between 2–5 days after ingestion of contaminated material, last between 7–10 days, and are usually flu-like in nature: acute diarrhea, fever, nausea, and vomiting. Because the bacteria occurs as a natural part of the normal flora of domestic animals like cattle and poultry, raw or undercooked meat (especially chicken) is a frequent source of foodborne Campylobacter illness in home kitchen settings (Blackburn and McClure 2009). Other vehicles of infection include contaminated water, raw or unpasteurized milk, and salad vegetables. Cross-contamination due to inadequate hygiene practices within the kitchen is a high risk factor for contracting Campylobacter
Risk Reduction Requires Knowledge and Behavior Change
Even though the number of foodborne illness cases occurring in domestic settings appears to be decreasing, educating consumers about home food safety is of the utmost importance (Scott 2003). Having insufficient knowledge of the risks associated at each level of food preparation can increase the number of incidents of foodborne illnesses at home (Collins 1997). Yet, the correlation between knowledge of proper hygiene practices and actual hygienic behavior in the home kitchen is still low among consumers (Worsfold and Griffith 1997).
The most common food-safety handling mistakes that occur within the household are improper food storage, inadequate cooking or reheating temperatures, cross- contamination, and infected food handlers (Scott 2003). However, research has shown that maintaining good hygiene practices can greatly help reduce many of the occurrences of foodborne illnesses (Scott 1996).
Food Storage
Food must be stored in a manner that minimizes microbial growth. Cooked food should be stored in the refrigerator below 41°F or in the freezer below 0°F (FDA 2013). Because refrigeration does not completely eliminate the potential growth of pathogenic bacteria, leftover food stored in the refrigerator should be consumed or discarded within 3 to 5 days. Expiration dates for foods should also be checked regularly. Frozen food should be thawed either in the refrigerator until ready, under cold running water (below 70°F), or in a microwave oven (FDA 2013). Raw foods and cooked foods should be stored separately in the refrigerator in order to prevent cross-contamination between the two. Furthermore, each item should be covered or wrapped (FDA 2013).
Cooking and Reheating
In the prevention of microbial growth, proper cooking of food is equally important. All cooking equipment (e.g., ovens and microwaves) should be used as instructed in the manufacturer's guide and should be maintained and cleaned (FDA 2013). Internal cooking temperatures should reach and sustain the safe minimum as recommended in Table 1 and should be checked with the appropriate food thermometer in accordance with these latest USDA guidelines.
Keeping It Clean
High-risk sources of cross-contamination in the kitchen include hands and food-contact surfaces such as cutting boards and counter tops (FDA 2013). It is very important to adequately wash hands with warm, soapy water and a sanitizing solution before handling food, before eating, after using the restroom, after handling a pet or child, and after contact with raw meat or other high-risk food items. The use of a dishwasher has been found to be more effective in reducing contamination of cutting boards and flatware than by washing by hand (FDA 2013).
Resources for Educators
Healthy People 2020, an initiative set forth by the US Department of Health and Human Services (HHS), has already begun to outline objectives that will improve these food safety practices among consumers (DOH 2011). These objectives (Figure 1) aim to increase the number of people who wash hands and food contact surfaces (CLEAN), do not cross-contaminate (SEPARATE), cook to adequate temperatures (COOK), and refrigerate promptly (CHILL). Thus, adequate hygiene factors are the basis of many educational and assistance programs aimed at improving food safety in home kitchen settings. Each of these food-safety goals can be traced back to the general conclusion that prevention of foodborne illness occurs through proper food preparation and sanitation techniques (Collins 1997).
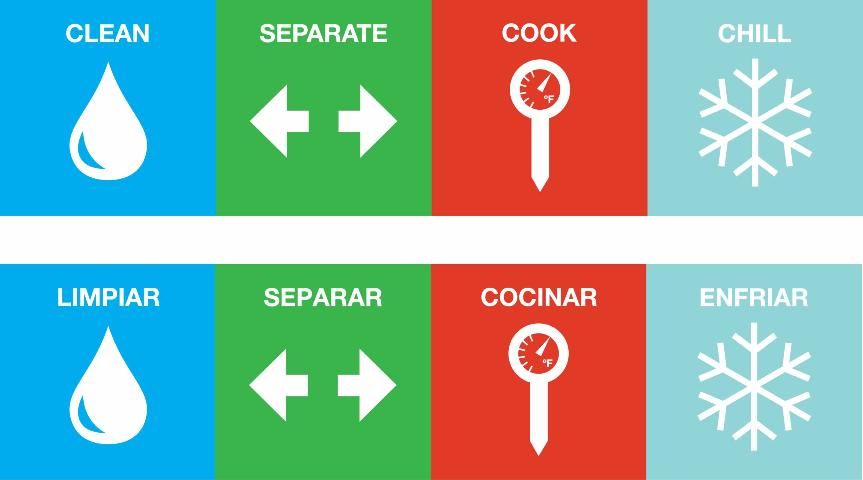
Credit: http://www.healthypeople.gov/
The Partnership for Food Safety Education is a non-profit organization that works to eliminate illness and death from foodborne disease through various educational campaigns. It was established in 1997 in response to a need for increased awareness of food safety among consumers (especially among at-risk populations including pregnant women, young children, the elderly, and the immuno-compromised). Food-safety education campaigns such as "Fight BAC!" and "Be Food Safe" provide information on potential causes and associated costs of foodborne illness and promote lifestyle changes in accordance with preventative guidelines (The Partnership for Food Safety 2024).
Another campaign that began in 2011 is Food Safe Families. It is a collaboration between the USDA's Food Safety Inspection Service (FSIS), the US Food and Drug Administration (FDA), and the Centers for Disease Control and Prevention (CDC). Its aim is to raise awareness about foodborne illness and encourage consumers to make lifestyle changes that lower their risk of contracting foodborne illness and practice safe food-handling techniques. The target audiences are English- and Spanish-speaking families who cook at least four times a week (USDA-FSIS 2011).
Closing Remarks
Although food-safety education is well established, people continue to be affected by foodborne illnesses associated with unsafe food handling at home. Many individuals just might not be aware of the potential risks associated with certain food-handling practices. Additionally, individuals with adequate knowledge of food-safety practices might not always apply these standards in home-kitchen settings. Because of these risks, the Healthy People seeks to educate consumers about foodborne illness in a manner that promotes harm-reducing lifestyle changes (DOH 2011).
References
Bell, C., and A. Kyriakides. 2009a. "Salmonella." Foodborne Pathogens—Hazards, Risk Analysis and Control, 2 ed., Clive de W. Blackburn and Peter J. McClure, eds., 581–674. Cambridge: CRC Press/Woodhead Publishing Limited. Accessed on December 5, 2024. https://www.sciencedirect.com/book/9781845693626/foodborne-pathogens
Bell, C., and A. Kyriakides. 2009b. "Pathogenic Escherichia coli. "Foodborne Pathogens—Hazards, Risk Analysis and Control, 2 ed., Clive de W. Blackburn and Peter J. McClure, eds., 581–674. Cambridge: CRC Press/Woodhead Publishing Limited. Accessed December 5, 2024. https://www.sciencedirect.com/book/9781845693626/foodborne-pathogens
Blackburn, C. de W., and P. J. McClure. 2009. "Campylobacter and Arcobacter." Foodborne Pathogens—Hazards, Risk Analysis and Control, 2 ed., Clive de W. Blackburn and Peter J. McClure, eds., 581–674. Cambridge: CRC Press/Woodhead Publishing Limited. Accessed December 5, 2024. https://www.sciencedirect.com/book/9781845693626/foodborne-pathogens
Collins, J. E. 1997. "Impact of changing consumer lifestyles on the emergence/reemergence of foodborne pathogens." Emerging Infectious Diseases. 3(4): 471–79. Accessed December 5, 2024. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2640078/pdf/9366599.pdf.
Department of Health and Human Services (DOH), Healthy People 2020. Office of Disease Prevention and Health Promotion, Washington, DC. Accessed December 5, 2024. http://www.healthypeople.gov/
Grass, J., L. H. Gould, and B. E. Mahon. 2013. "Epidemiology of Foodborne Disease Outbreaks Caused by Clostridium perfringens, United States, 1998–2010." Foodborne Pathogens and Disease. 10(2): 131–135. Accessed December 5, 2024. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4595929/
Heiman, K., R. K. Mody. S. D. Johnson, P. M. Griffin, and L. H. Gould. 2015. "Escherichia coli O157 Outbreaks in the United States, 2003–2012." Emerging Infectious Diseases 21(8): 1293–1301. Accessed October 9, 2015. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4517704/
Jensen, D., L. M. Friedrich, L. J. Harris, M. D. Danyluk, and D. W. Schaffner. 2015. "Cross contamination of Escherichia coli O157:H7 between lettuce and wash water during home-scale washing." Food Microbiology. 46: 428–433. Accessed December 5, 2024. http://www.sciencedirect.com/science/article/pii/S0740002014002330
The Partnership for Food Safety Education. 2024. Fight BAC!® Keep Food Safe from Bacteria. Accessed December 5, 2024. http://www.fightbac.org
Radford, S., and R. G. Board. 1993. "Review: Fate of pathogens in home-made mayonnaise and related products." Food Microbiology. 10: 269–278. Accessed December 5, 2024. https://www.sciencedirect.com/science/article/pii/S0740002083710312
Scallan, E., R. M. Hoekstra, F. J. Angulo, R. V. Tauxe, M. A. Widdowson, S. Roy,. L. J. Jones, and P. M. Griffin. 2011. "Foodborne illness acquired in the United States—major pathogens." Emerging Infectious Diseases. 17(1): 7–15. doi: 10.3201/eid1701.p11101
Scott, E. 2003. "Food safety and foodborne disease in 21st century homes." The Canadian Journal of Infectious Diseases 14(5): 277–80. Accessed December 5, 2024. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2094945/pdf/JID14277.pdf
US Centers for Disease Control and Prevention (CDC). 2024. "Norovirus: Facts for Food Workers." National Center for Immunization and Respiratory Diseases, Division of Viral Diseases. Accessed December 5, 2024. https://www.cdc.gov/norovirus/communication-resources/facts-for-food-workers.html
US Centers for Disease Control and Prevention (CDC). 2013. "Tracking and Reporting Foodborne Disease Outbreaks." Data & Statistics. Accessed October 9, 2015. http://www.cdc.gov/features/dsfoodborneoutbreaks/index.html
US Centers for Disease Control and Prevention (CDC). 2011. "CDC 2011 Estimates: Findings." CDC Estimates of Foodborne Illness in the United States. Accessed December 5, 2024. http://www.cdc.gov/foodborneburden/2011-foodborne-estimates.html
US Food and Drug Administration (FDA). 2013. "Food Code 2013."U.S. Public Health Service. Accessed December 5, 2024. http://www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf
United States Department of Agriculture-Food Safety Inspection Service (USDA-FSIS). 2011. Food Safe Families: First-Ever National Multimedia Food Safety Campaign Launches to Reduce Food Poisoning in the U.S. Accessed December 5, 2024. https://www.usda.gov/media/blog/2011/06/28/food-safe-families-first-ever-national-multimedia-food-safety-campaign
Worsfold, D., and C. Griffith. 1997. "Food safety behaviour in the home." British Food Journal. 99(3): 97–104. Accessed December 5, 2024. https://doi.org/10.1108/00070709710168932