Mange is a persistent skin condition of mammals caused by infestation with parasitic mites. Mites are tiny arthropods, usually less than 1 mm in length and difficult to see with the naked eye. Adult mites have eight legs, and larvae have six. The effect of the mites on the animal's skin, called "mange," is the most visible sign of an infestation.
There are two types of mites that cause mange: burrowing and non-burrowing mites. Female burrowing mites tunnel into the animal's skin and lay their eggs. Non-burrowing mites typically invade hair follicles and glands or live on the surface of the skin. The symptoms of mange are redness and itching of the skin as well as hair loss. The irritation of the skin is due to an allergic response to molecules associated with the mite's bodies, secretions (e.g., saliva), and fecal material.
Several skin conditions commonly caused by parasitic mites in domestic animals are described below, including sarcoptic, notoedric, demodectic, otodectic, and psoroptic mange. Of these forms of mange, only sarcoptic and notoedric mange are caused by female mites burrowing in the skin. Sarcoptic mange commonly occurs in dogs and notoedric mange in cats. Mange can afflict humans, horses, sheep, cattle, and other animals. Mange-causing mites spread through direct contact from infested to non-infested animals; however, the development and severity of mange will depend upon the type of mite and the animal's health. Temporary animal mange may be contracted by the owners and handlers of infested animals, although this is typically limited to the burrowing mites that cause sarcoptic and notoedric mange. Humans are not appropriate hosts for these mite species, and infestations in humans are short-lived because the mites do not form burrows or reproduce in human skin. When a cat or dog is treated, any reactions in humans who have contact with the animal will clear up quickly.
Types of Mange and Mange-Causing Mites
Sarcoptic Mange
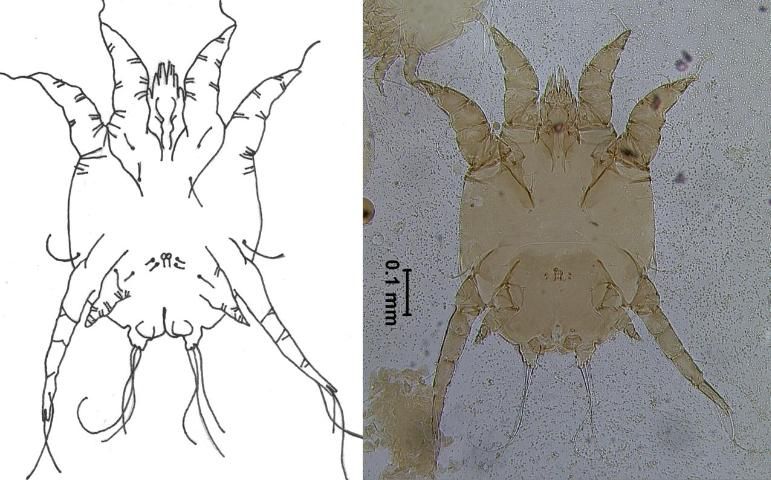
Sarcoptic mange occurs in all domestic animals except cats and guinea pigs, but is most common in dogs. The related condition in humans is called scabies. Mange in dogs is caused by the canine mange mite (Figure 1), which frequently also attacks humans, causing temporary infestations. Wild canids, e.g., red fox, gray fox, wolf, and coyote, are particularly susceptible to the canine mange mite. Domesticated dogs may be infested through contact with infested domestic or wild canids.
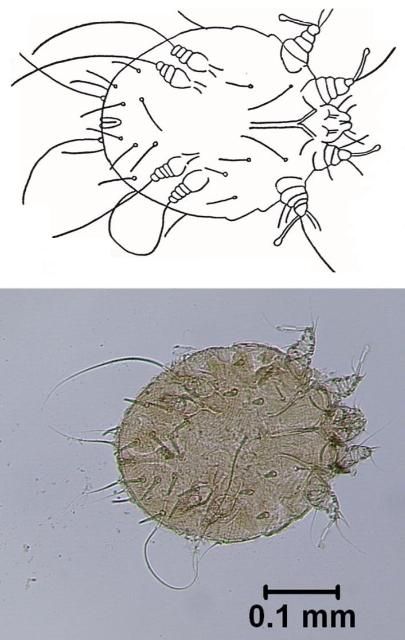
Credit: E. N. I. Weeks, UF/IFAS
All stages of the canine mange mite live in burrows in the skin formed by tunneling female mites. Female mites lay up to three eggs a day for two to three weeks in these burrows. The eggs hatch in three to five days, and the larvae molt to the nymphal stage. The nymphs mature to adults, and then the adults mate on the surface of the skin. The whole life cycle from egg to adult is completed within two to three weeks.
The skin reaction in the animal is caused by the presence of the mites and their excrement in the burrows. The first symptoms usually appear three weeks after the animal becomes infested, although the delay decreases with repeated exposures. The lesions start where the hair is thin, most commonly on the head, and then spread across the animal. The skin becomes itchy and erupts in red, inflamed papules (wart-like growths), and the animal's hair falls out (Figure 2). The burrowing mites cause the skin to ooze serum, which dries and forms crusty scabs. Scratching spreads the infestation and often leads to secondary infection of wounds. These infections cause the unpleasant odor often associated with "mangy" animals. Infested animals may suffer from weight loss, lack of appetite, and poor hearing and vision. If the mange is left untreated, animals may die of exhaustion or dehydration or as the result of a secondary infection.

Credit: Department of Pathobiology, College of Veterinary Medicine, Auburn University
The canine mange mite is specific to dogs, yet human infestations of dog handlers or owners are common. These temporary infestations result from contact with infested dogs and are known as "animal scabies." The symptoms in humans are pimples or blisters and inflammation on the forearms, thighs, and abdomen. Because the skin reaction is due to an immune response to the mites rather than to the mites themselves, the symptoms may occur in areas that are not infested with mites. Some individuals will react more severely than others depending on various factors including previous exposure.
Notoedric Mange
Notoedric mange is caused by the most common mite of domestic cats in North America, Europe, and Africa, Notoedres cati (Figure 3). This mite occurs on cats (wild and domesticated), rats, squirrels, rabbits, and bats. Notoedric mites rarely infest dogs or other canids, but they occasionally and temporarily infest humans.
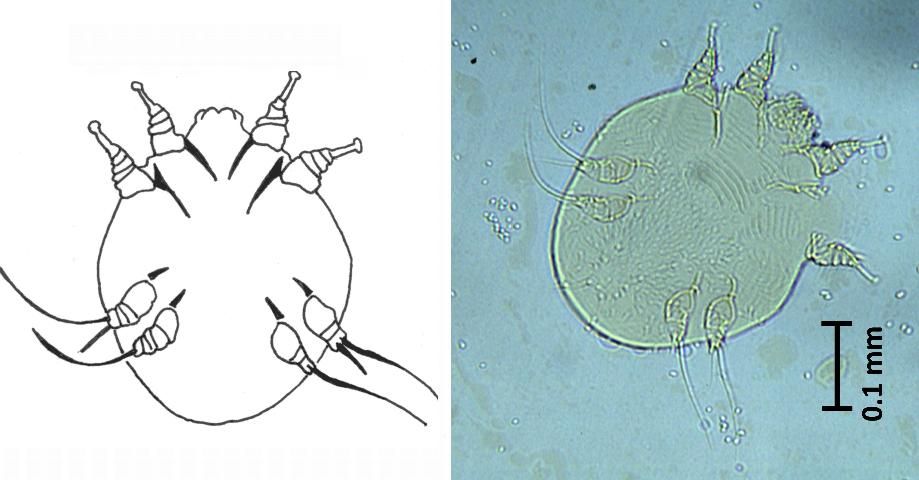
Credit: J. F. Butler (photo); E. N. I. Weeks (illustration), UF/IFAS
Even under a microscope these mites appear very similar to the Sarcoptes mites, but there are differences that can be used to tell the two apart using a compound microscope and identification keys. The adult female notoedric mite burrows in the skin and deposits eggs, which hatch after three to four days. The entire life cycle from egg to adult takes just 6–10 days. The females also may invade hair follicles or sebaceous glands.
Symptoms of notoedric mange usually begin on an animal's head, in particular the ears, face, neck, and shoulders. The irritation is intense, with reddening, scaling, hair loss, and formation of gray/yellow crusts (Figure 4). The infested skin becomes thick, folded, and wrinkled. The irritation causes the animal to scratch, resulting in removal of skin and further irritation. Chronic cases may lead to debilitation and death.

Credit: Department of Pathobiology, College of Veterinary Medicine, Auburn University
Human beings may contract temporary notoedric mange through contact with infested animals. The most common sites of skin lesions in humans are the legs and hands—the areas most likely to be in contact with an infested animal. Prolonged exposure to the mite causes sensitization in humans. Once sensitized, a person may experience an exaggerated immune response such as intense itching after just a few hours of exposure, even though the mites do not burrow into human skin.
Demodectic Mange
Demodectic mange is caused by mites living in the hair follicles or associated sebaceous glands of mammals (Figure 5). Dogs, livestock, wild animals, and laboratory animals are commonly infested; the mite is uncommon in cats and horses. Each animal has its own species of mite, and infestation of one species by another species' mite is rare. Transmission of the mites may occur from mother to offspring during the first few days of life through nursing. The eggs and all the life stages of these mites are found in the hair follicles or glands, and the full life cycle occurs in three to four weeks.
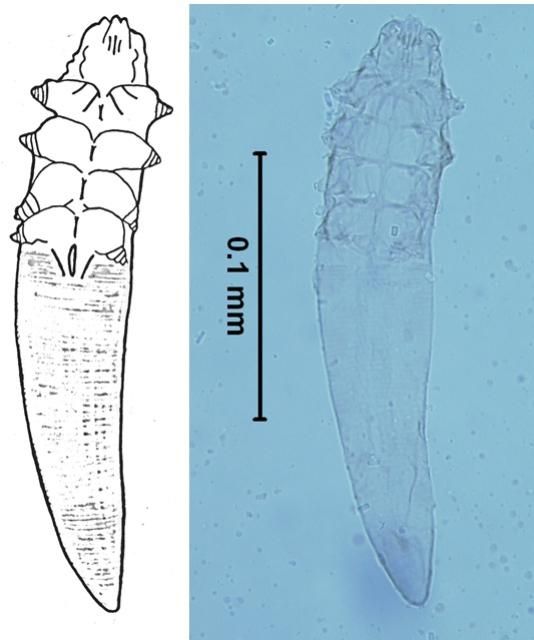
Credit: E. N. I. Weeks, UF/IFAS
Healthy animals experience only mild and temporary deterioration in skin condition, if they show any symptoms at all. Clinical symptoms are most common in dogs, particularly young animals (less than one year old), or animals with weak immune systems; in such animals the irritation caused by the mites may lead to a dangerous generalized demodicosis (Figure 6a) and the development of red mange (a severe irritation; Figure 6b). Certain breeds of dog are more susceptible to demodectic mange, including Old English sheepdogs, collies, Afghan hounds, German shepherds, Akitas, Doberman pinschers, English bulldogs, Great Danes, dachshunds, Chihuahuas, chow chows, boxers, pugs, Chinese shar-peis, beagles, pointers, and many terrier breeds including American Staffordshire terriers, American pitbull terriers, English bull terrier, miniature bull terrier, West Highland terrier, rat terrier, and Boston terriers. Symptoms in other animals are rare, though cats and horses may develop mild demodectic mange, usually localized and self-limiting. Siamese and Burmese cat breeds are more susceptible to generalized demodicosis.

Credit: J. F. Butler, UF/IFAS
Canine demodectic mange usually appears as red, bald patches around the eyes and mouth. The mites and the associated mange may spread to the front legs and trunk. In most cases the animal's immune system will defeat the infestation without treatment, but in some animals, such as those with a genetic predisposition or a depressed immune system, the symptoms may become severe. A condition called pustular demodicosis may develop, in which pus-filled swellings form on the skin. These can become infected and give off an unpleasant odor from the bacterial infection. The smell is often described as "rancid" or "mousy." If the irritation becomes generalized and the skin becomes intensely red and tender and bleeds easily, then the condition is known as red mange. The condition usually starts on the head and face but will quickly spread to the rest of the body. If the animal is not treated, its immune system will weaken, and it will eventually be killed by a secondary infection.
Otodectic Mange
Ear mange, caused by the otodectic ear mite, is common among cats and dogs (Figure 7). The mites also infest the ears of other carnivores such as foxes and raccoons.
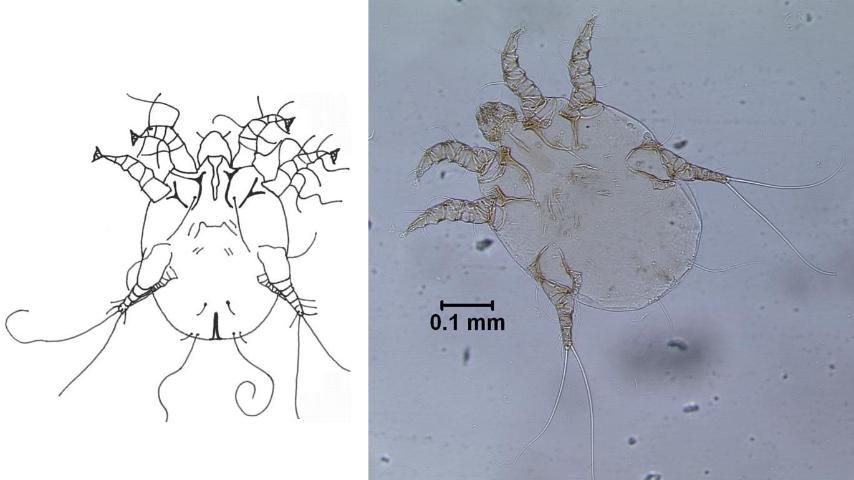
Credit: E. N. I. Weeks, UF/IFAS
All of the otodectic mite's life stages are found within the ear canal, though in some cases otodectic infestations can spread beyond the ear to the rest of the body, particularly the head, tail, and feet. Otodectic mites do not burrow into the skin, living instead on skin surfaces deep inside the external ear canal. These mites feed primarily on skin but occasionally pierce the skin to feed on blood, serum, and lymph.
The feeding mites cause injury because the skin inside the ear swells and blocks follicles and glands, causing the formation of papules and nodules. Hair falls out and secondary infections may develop. The ear canal becomes congested, often resulting in hearing loss. Infested animals will be seen to shake their heads and rub their ears in an attempt to relieve the itching. The responses in animals are highly variable from asymptomatic, to severe otitis, to convulsive seizures (particularly in cats).
Psoroptic Mange
Psoroptic mange mites occur in the ears of domestic and wild animals, particularly rabbits (Figure 8). These ear mites do not burrow. Instead they feed on skin tissue, which irritates the skin and causes lesions. The lesions produce scabs, and the scabs protect the mites from the environment and shield them from removal by the animal when it scratches.
Credit: E. N. I. Weeks, UF/IFAS
All of the developmental stages of these mites will be found under scabs in the ear canal. Eggs laid by the female mite hatch within four days; the life cycle takes a total of three weeks from egg to adult.
Symptoms start in the external ear canal, with loose crusts and brown, strong-smelling discharge becoming evident (Figure 9). The animal will show characteristic behavior: scratching, shaking its head, losing its balance, and tensing its neck muscles. The infestation may spread to other parts of the body, and the lesions may become infected with bacteria.

Credit: Department of Pathobiology, College of Veterinary Medicine, Auburn University
Prevention
Prevention of mange involves the promotion of good health and hygiene to enhance resistance against mites and mite-induced skin diseases. Canine mange mainly occurs in young animals in poor condition; for example, malnourished puppies or those that are suffering with a secondary condition such as internal parasite infection. Puppies that are mothered by mite-infested animals also will be at increased risk. As direct contact is the most important method of transmission, pets with mange should be quarantined. Healthy animals should not be permitted to have contact with mangy animals or with areas previously occupied by mangy animals.
In order to avoid passing on the genetic predisposition for severe mange, an animal that has suffered with demodectic mange should not be used for breeding, particularly if the animal developed secondary complications (e.g., red mange). Severity of the disease depends on each animal's individual level of immune response to the mite. Some animals have been shown to have a genetic predisposition to an elevated immune response and are, therefore, more likely to develop pustular demodicosis or red mange.
Treatment
In almost all cases of mange on domestic animals, a veterinarian should be consulted. An owner or handler suspecting mange should take the animal to a veterinarian for diagnosis and treatment. Because mange-like symptoms can manifest in response to stress or to other allergens such as flea bites, it is particularly important to get an accurate diagnosis. Mange is usually diagnosed by the detection of the mites in the affected area. For example, skin scrapes are done for most types of suspected mange. PCR of skin scrapes for presence of S. scabiei DNA is a reliable method of detecting infestations, particularly in the early stages of an infestation when microscopy of skin scrapes may produce false negatives. Although animals will usually self-cure from demodectic mange, it is advisable to get a diagnosis from a veterinarian in case secondary complications develop such as pustular demodicosis and red mange.
Treatment for Animals
Treatment of most mange mites involves three steps:
- Isolation of the animal to prevent spread to non-infested individuals.
- Medication to kill the mites.
- Treatment of the animal's environment.
The veterinarian will prescribe either a topical or an internal miticide. Topical medications include creams, shampoos, and dips; internal preparations are either given orally or injected. The veterinarian also may prescribe medications to ease the itching or to treat bacterial infections. It may be necessary to clip long-haired animals to ensure success of topical treatments. All animals in the house at risk of infestation should be treated at the same time, whether they are symptomatic or not. It is important that any prescribed drugs are used for the specified treatment period, and not discontinued early if the symptoms begin to ease. Asymptomatic ear mange can be treated at home by the application of mineral oil to the ear canal with a medicine dropper or a cotton swab. The outer ear should be cleaned to remove accumulations of material every other day for about three weeks.
Treating the environment is important, and particularly so in cases of sarcoptic mange. Wash all bedding and clothing in hot, soapy water, and dry at hot temperatures. Wash or replace collars. If the pet stays indoors, the veterinarian may advise an indoor carpet and furniture treatment.
Treatment for Humans
Humans with animal mange-like symptoms should consult a physician for diagnosis and treatment and take their pets to the veterinarian if they themselves are found to be infested. Sarcoptic mange is the usual condition found in humans that have been exposed to infested dogs, but notodectic mange from exposure to infested cats is also possible, particularly in children or in individuals with a weakened immune system. In humans, infestation with animal mites is temporary, and the mites do not burrow in the skin or reproduce. Therefore, if the companion animal is treated then the symptoms in the owners and handlers will resolve.
Selected References
Chakrabarti, A. 1986. "Human notoedric scabies from contact with cats infested with Notoedres cati." Int. J. Dermatol. 25: 646–64. https://doi.org/10.1111/j.1365-4362.1986.tb04527.x
Fraser, T. A., A. Martin, A. Polkinghorne., and S. Carver. 2018. "Comparative diagnostics reveals PCR assays on skin scrapings is the most reliable method to detect Sarcoptes scabiei infestations." Vet. Parasitol. 251: 119–124. https://doi.org/10.1016/j.vetpar.2018.01.007
Mullen, G. R., and B. M. OConnor. 2009. Mites (Acari), pp. 433–492. In G. R. Mullen and L. A. Durden (eds.), Medical and Veterinary Entomology vol. 2. Elsevier, Burlington, MA, USA.
Nutting, W. B. 1976. "Hair follicle mites (Demodex spp.) of medical and veterinary concern." Cornell. Vet. 66: 214–231.
Rafferty, D. E., and J. S. Gray. 1987. "The feeding behaviour of Psoroptes spp. mites on rabbits and sheep." J. Parasitol. 73: 901–906. https://doi.org/10.2307/3282508
Stone, W. B., E. Parks, B. L. Weber, and F. J. Parks. 1972. "Experimental transfer of sarcoptic mange from red foxes and wild canids to captive wildlife and domestic animals." New York Fish Game J. 19: 1–11.
Sweatman, G. K. 1958a. "Biology of Otodectes cynotis, the ear canker mite of carnivores." C. J. Zool. 36: 849–862. https://doi.org/10.1139/z58-072
Sweatman, G. K. 1958b. "On the life history and validity of the species in Psoroptes, a genus of mange mites." C. J. Zool. 36: 905–929. https://doi.org/10.1139/z58-078
Walker, E. D., and J. A. Stachecki. 1994. Mites and Ticks, pp. 93–104. In Pest management for small animals: A training manual for commercial pesticide applicators and registered technicians (Category 7G), Michigan State University Extension, Michigan. https://www.canr.msu.edu/ipm/uploads/files/TrainingManuals_SmallAnimals/SmallAnimals_Whole.pdf (18 Dec 2018).
Whitaker, J. O. 1982. Ectoparasites of mammals of Indiana. The Indiana Academy of Science, Indianapolis, Indiana. http://phthiraptera.info/content/ectoparasites-indiana (18 Dec 2018).