Lyme disease was first documented in the United States in 1975. The organism that causes Lyme disease is transmitted by the bite of a tick. Lyme disease is named for the town in Connecticut where some of the first cases occurred in the United States. Lyme disease cases have since been documented in about 43 states, with over 15,000 cases reported annually between 1998 and 2004. Over 153,000 total cases were reported in the United States between 1993 and 2002. During 2002, 23,763 Lyme disease cases were reported, making this the peak year. During 2003-2005, 64,382 cases were reported. During the year of 2007, 27,444 cases of Lyme disease were reported, yielding a national average of 9.1 cases per 100,000 persons. Several cases of Lyme disease have been reported in Florida as well, corresponding to approximately 40 cases per year.
The primary vector of Lyme disease in the United States is the black-legged deer tick (Figures 1 and 2). Other closely related ticks are also known to transmit the disease. Lyme disease is maintained in wild rodent populations, on which the larval and nymphal ticks develop. These immature ticks pick up the disease organism when they suck the blood of infected rodents. The nymphal and adult ticks then seek a larger host, such as deer or humans, to obtain their final blood meal and transmit the disease when they feed.
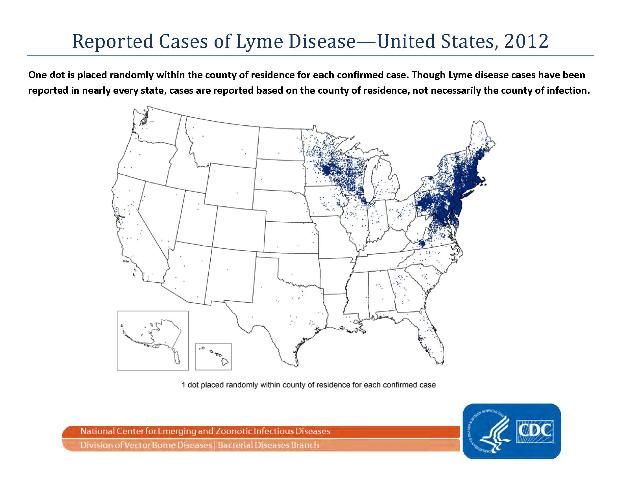
Credit: Centers for Disease Control

Credit: J. F. Butler, UF/IFAS
Symptoms
The first sign of Lyme disease in 70%-80% of patients is a red circular rash, called an erythema migrans, around the puncture mark made where the tick pierced the skin. This rash appears after a three-to-30 day delay. The most common shape of the rash is an oval 2- to 3-inches in diameter that usually lasts about four weeks. The center of the rash occasionally will lighten resulting in a bull's-eye appearance. The rash does not itch but may feel warm to the touch. Some patients might develop additional lesions in other parts of their body. Flu-like symptoms may also develop that often include aches, fever, fatigue, muscle pain, joint pain, and headache. Arthritis, cardiac disease, and neurologic disorders may develop if the disease is not properly or promptly treated. Sometimes these more serious symptoms develop without the individual ever having had a rash.
A different but similar disease occurs in Florida, and this disease is often confused with Lyme disease. Southern tick-associated rash illness is caused by a pathogen that is closely related to Lyme disease and vectored by the lone star tick. This disease was first reported in 2001 and occurs wherever lone star ticks are found. Similar to Lyme disease, a red, expanding rash with a central, clear area at the site of the tick bite has been reported.
Treatment
Once diagnosed, Lyme disease can be treated. Physicians can determine if an individual has been infected by the Lyme disease organism using a simple blood test; however, some people test negative but have the disease. The CDC warns against unproven tests, and proper testing procedures are important.
Infection can be treated by taking certain antibiotics. However, no immunity is conferred from infection so a person could get Lyme disease again from another infected tick.
Pets and other animals can contract Lyme disease as well, exhibiting symptoms similar to those in humans. Veterinar ians can test for Lyme disease in pets and domestic animals exhibiting suspicious signs of arthritis (in younger animals), heart problems, or neurological signs.
Antibiotics used for treatments of Lyme disease include doxycycline, amoxicillin, or cefuroxime axetil. When patients are treated early in the stages of infection they recover fast and completely. Patients diagnosed with later symptoms of the disease may have persistent or recurrent symptoms even when treated.
Prevention
The best prevention against Lyme disease is to avoid being bitten by ticks. Individuals who spend a lot of time out- doors should be aware of the danger and make it a habit to regularly check their bodies for ticks. The tick requires time to attach itself and begin feeding. It is possible to remove ticks before they are able to transmit the disease. Ticks should be grasped with tweezers at the point where their mouthparts enter the skin and pulled straight out with firm pressure. Immature ticks are small and difficult to detect; often they appear as a freckle or mole.
Stay out of dense undergrowth unless absolutely necessary. Walk on closely mowed grass or paved walkways whenever possible.
Wear long-sleeved shirts and long pants tucked into socks. Light-colored clothes make ticks more visible and easier to pick off.
Apply tick repellent to socks and shoes to prevent ticks from crawling onto clothing.
Inspect yourself and others thoroughly after walking through areas suspected of being infested with ticks.
When taking children on nature outings, keep them in a group with a leader who knows to avoid tick-infested areas and can inspect them for ticks.
See a doctor if Lyme disease symptoms appear.
A Lyme disease vaccine was withdrawn from the market, reportedly due to poor sales.
Tick Control
Recommendations for control of ticks include:
-
Keep grass cut low to reduce humidity and thus kill ticks.
-
Discourage wild animals (raccoons, skunks, deer, mice, etc.) from coming around your yard. They often harbor the ticks that transmit Lyme disease. Area treatment with insecticides is not warranted in most cases. However, in some situations it might be appropriate to use insecticides for control of ticks. Check with your local UF/IFAS Extension office for current UF/IFAS recommendations.
References
Anderson, JF, LA Magnarelli, W Burgdorfer, and AG Barbour. 1983. Spirochetes in Ixodes dammini and mam- mals in Connecticut. Am. J. Trop. Med. Hyg. 32: 818–24.
Barbour, AG and D Fish. 1993. The biological and social phenomenon of Lyme disease. Science. 260. 1610–16.
Burgdorfer, W, AG Barbour, SF Hayes, JL Benach, E Grunwaldt, and JP Davis. 1982. Lyme disease—a tick-borne spirochetosis? Science. 216: 1317–19.
Daniels, TJ, D Fish, JF Levine, MA Greco, AT Eaton, PJ Padgett, and DA LaPointe. 1993. Canine exposure to Bor- relia burgdorferi and prevalence of Ixodes dammini (Acari: Ixodidae) on deer as a measure of Lyme disease risk in the northeastern United States. J. Med. Entomol. 30: 171–78.
Coyle, BS, GT Strickland, YY Liang, C Pena, R McCarter, and E Israel. 1996. The public health impact of Lyme disease in Maryland. J. Infect. Dis. 173: 1260–62.
Hayes, EB and J Piesman. 2003. How can we prevent Lyme disease? N. Engl. J. Med. 348: 2424–30.
Mather, TN, JMC Ribeiro, SI Moore, and A Spielman. 1988. Reducing transmission of Lyme disease spirochetes in a suburban setting. Ann. New York Acad. Sci. 539: 402–03.
Meek, JI, CL Roberts, EV Smith Jr, and ML Cartter. 1996. Underreporting of Lyme disease by Connecticut physicians. 1992. J. Public. Health Manage. Pract. 2: 61–65.
Pound, JM, JA Miller, JE George, and CA Lemeilleur. 2000. The `4-poster' passive topical treatment device to apply acaricide for controlling ticks (Acari: Ixodidae) feeding on white-tailed deer. J. Med. Entomol. 37: 588–94.
Shulze, TL, WM McDevitt, WE Parkin, and JK Shisler. 1987. Effectiveness of two insecticides in controlling Ixodes dammini (Acari: Ixodidae) following an outbreak of Lyme disease in New Jersey. J. Med. Entomol. 24: 420–24.
Schulze, TL, RA Jordan, and RW Hung. 1995. Suppression of subadult Ixodes scapularis (Acari: Ixodidae) following removal of leaf litter. J. Med. Entomol. 32: 730–33.
Schulze, TL, RA Jordan, RW Hung, RC Taylor, D Markowski, and MS Chomsky. 2001. Efficacy of granular deltamethrin against Ixodes scapularis and Amblyomma americanum (Acari: Ixodidae) nymphs. J. Med. Entomol. 38: 344–46.
Stafford, KC. 1991. Effectiveness of carbaryl applications for the control of Ixodes dammini (Acari: Ixodidae) nymphs in an endemic residential area. J. Med. Entomol. 28: 32–36.
Steere, AC, E Taylor, GL McHugh, and EL Logigian. 1993. The overdiagnosis of Lyme disease. JAMA. 269: 1812–16.
Wormser, GP, RB Nadelman, RJ Dattwyler, DT Dennis, ED Shapiro, AC Steere, TJ Rush, DW Rahn, PK Coyle, DH Persing, D Fish, and BJ Luft. 2000. Practice guidelines for the treatment of Lyme disease. Clinic Infect. Dis. 31: 1–14.