Abstract
Environmental heat is a leading cause of death from natural weather or environmental factors. In this study, we analyzed the data from Florida Vital Statistics to identify heat-related fatalities that occurred from 2010 to 2020 in Florida. Over the study period, there were 215 deaths related to environmental heat. Twenty-seven percent of these fatalities were in the age group of 65 and older. Prevention of heat-related deaths requires public education campaigns on heat-related hazards.
Introduction
Natural heat exposure is a continuing public health concern. Future increases in heat-related mortality are projected due to climate change (Petkova et al. 2017). In the United States, an average of 702 people died from exposure to natural extreme heat annually from 2004 to 2018 (Vaidyanathan 2020).
Heat-related death is defined as a death in which exposure to high ambient temperature either caused the death or significantly contributed to it (Donoghue 1997). According to the Centers for Disease Control and Prevention, extreme heat is defined as temperatures that are much hotter and/or more humid than average (CDC 2021). Heat-related illness (HRI), including heat cramps, heat exhaustion, or heatstroke, occurs when the human body is unable to adequately cool itself. People younger than 15 years or older than 65 years are highly affected by HRI. Similarly, people with medical conditions (e.g., heart disease, diabetes, previous heat injury, etc.) are susceptible to HRI.
Major risk factors for HRIs include drug and alcohol use, exposure to high temperatures and/or humidity, lack of acclimatization, age, obesity, and other medical conditions (Gauer and Meyers 2019).
This publication discusses heat-related deaths in Florida from 2010 to 2020 and presents safety recommendations as well as useful resources to prevent heat-related illnesses. This publication is intended for the public, especially children and older adults, athletes, and outdoor workers (farmers, construction laborers, landscaping workers, firefighters, law enforcement, forestry workers, etc.).
Methods
Summary information on death certificate data was obtained from the Bureau of Vital Statistics. Accidental deaths are classified by cause of death using The International Classification of Diseases, 10th Edition (WHO 2019). Heat-related deaths are identified by using the cause of death code X30 (exposure to excessive natural heat) and narrative text search terms by using “heat” and “sun.” The case narratives were reviewed to make sure they are all related to heat exposure. However, sometimes heat-related deaths are misclassified as another underlying cause (Weinberger et al. 2020). Thus, numbers represented in this report most likely underestimate the total number of heat-related deaths.
Results
From 2010 to 2020, 215 heat-related deaths occurred in Florida. The number of yearly deaths varied between 10 and 28 (Figure 1). Average temperatures over the study years (May to October—afternoon hours) aligned with the heat-related fatality trend (Dr. Ziwen Yu, unpublished study).
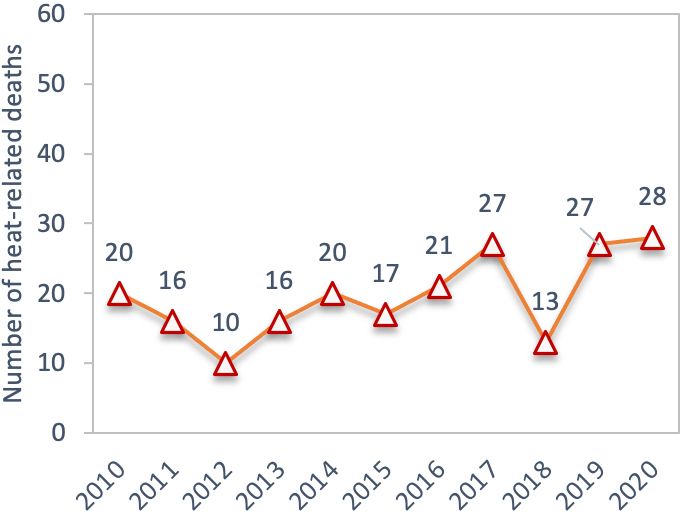
Credit: Serap Gorucu, UF/IFAS
Figure 2 shows heat-related fatalities by month. The highest number of fatalities occurred in June, followed by July and August. The fatalities that occurred from November through March include children who were left in a vehicle, victims who were in an enclosed place (vehicle or house), and other victims who were in a hot vehicle or hot enclosed place while intoxicated.
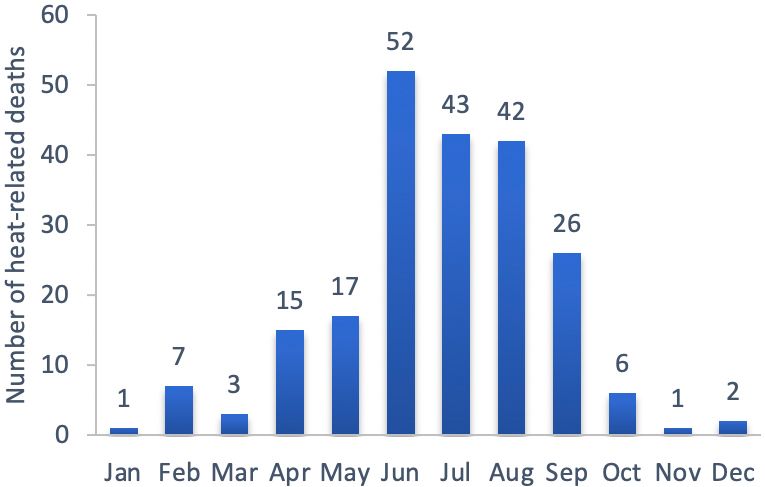
Credit: Serap Gorucu, UF/IFAS
The number of heat-related deaths varied by county (Figure 3). The highest numbers were found in the counties of Broward (10%), Miami-Dade (7%), Palm Beach (7%), Hillsborough (5%), Orange (5%), Brevard (5%), Duval (5%), Lee (4%), and Manatee (3%). Another 38 counties reported 1 to 5 heat-related deaths during the study period; however, county information was not available for 41 cases.
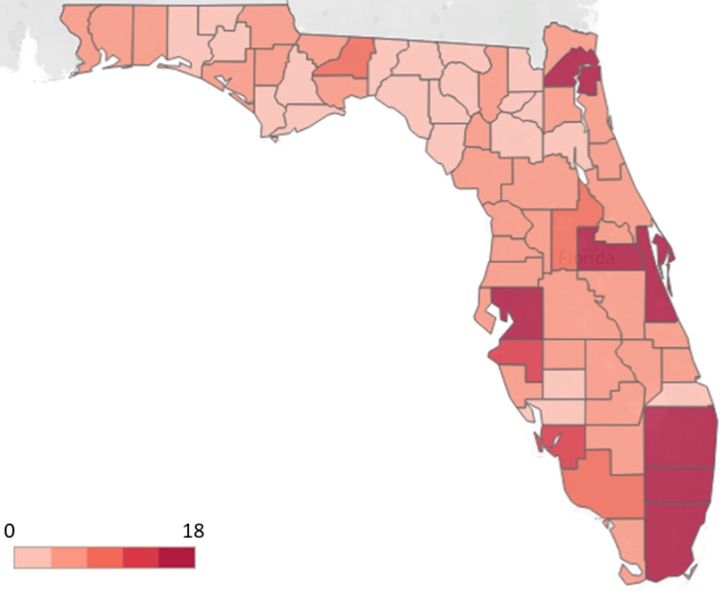
Credit: Serap Gorucu, UF/IFAS
Of the 215 fatalities, 153 (71%) were males and 62 (29%) were females. Victims’ ages ranged from 1 to 98. Older adults (65 and older) had the highest number of deaths (27%) (Figure 4). A total of 38 children died from heatstroke after being left in a vehicle. The age distribution in years for these victims is: 1 (n=15, 39%), 2 (n=10, 26%), 3–4 (n=7, 18%), and 5–11 (n=9, 24%). Four other victims under the age of 18 died during outdoor sports practices. Another child fatality had no information on the incident.
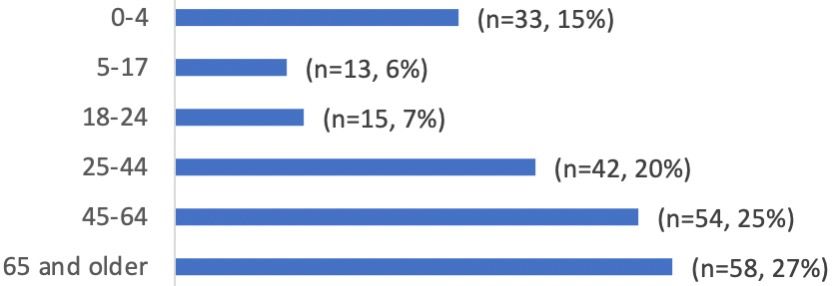
Credit: Serap Gorucu, UF/IFAS
For adults, there were 16 deaths caused by HRI with the added influence of drugs or alcohol. Another 16 victims died due to heat exposure in enclosed vehicles. Thirty-six of the remaining victims died during outdoor work. Other victims died due to excessive indoor heat (n=7), lethal sun exposure/sunbathing (n=7), and sports/exercise activities (n=4).
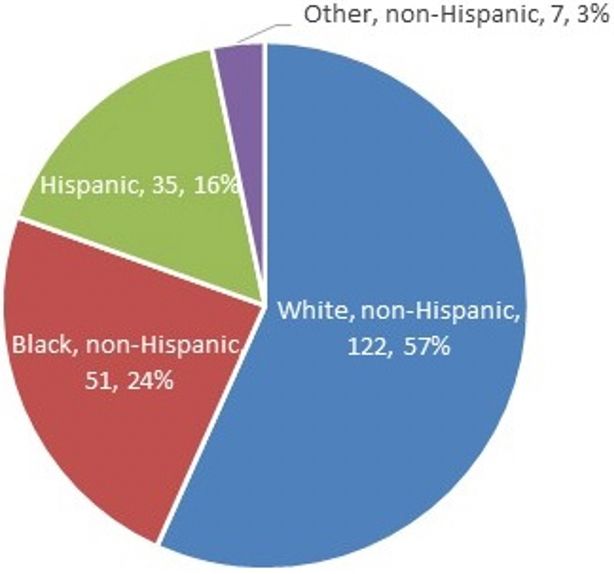
Figure 5 presents statewide heat-related deaths by race/ethnicity. Non-Hispanic whites (57%) comprised most of the deaths, followed by Black non-Hispanics (24%). When compared to Florida’s population distribution by ethnicity, the proportion of Hispanic and Black (non-Hispanic) individuals who die from heat exposure is higher than the state’s proportions (U.S. Census 2019).
Credit: Serap Gorucu, UF/IFAS
Safety Recommendations
Heat-related deaths and illnesses are preventable. Outdoor activities and confined spaces/vehicles in hot weather and high humidity can put people at risk for heat-related health problems and serious injuries. Some safety recommendations are given below.
- Do not leave children in vehicles: Florida has laws with specific language that addresses leaving a child unattended in a vehicle (The Florida Legislature 2020). A parent, legal guardian, or other person responsible for a child younger than 6 years of age may not leave the child unattended or unsupervised in a motor vehicle for longer than 15 minutes or for any period of time if the vehicle is running, or if the child is in distress or danger.
- Schedule/Limit outdoor activities: Try to limit outdoor activities to when it is cool (i.e., early morning or evening hours in well-shaded areas).
- Make healthy outdoor choices: Stay hydrated, drink plenty of nonalcoholic drinks, and stay in cool places. Avoid hot and heavy meals and strenuous outdoor sports. Wear sunscreen, hats, and light-colored, lightweight, loose-fitting clothing.
- Monitor people at risk: Young children and adults aged 65 and older, people with heart disease or high blood pressure, and people on certain medications are at greater risk.
- Avoid alcohol/drugs: Use of alcohol and drugs is a risk factor for heat-related deaths.
- Outdoor workers: Drink plenty of water, seek shade, and take breaks. If possible, reschedule or rearrange work schedules when there are high or extreme risk levels of HRI.
Resources
Below are a few resources on extreme heat and heat-related illness prevention.
- CDC: https://www.cdc.gov/disasters/extremeheat/index.html
- OSHA: https://www.osha.gov/heat-exposure
- OSHA-NIOSH Heat Safety Tool App: https://www.cdc.gov/niosh/topics/heatstress/heatapp.html
- Environmental Protection Agency (EPA): https://www.epa.gov/natural-disasters/extreme-heat
References
Donoghue, E. R., M. A. Graham, J. M. Jentzen, B. D. Lifschultz, J. L. Luke, and H. G. Mirchandani. 1997. “Criteria for the Diagnosis of Heat-Related Deaths: National Association of Medical Examiners: Position Paper.” The American Journal of Forensic Medicine and Pathology 18(1): 11–14.
The Florida Legislature. 2020. “The 2020 Florida Statutes.” http://www.leg.state.fl.us/Statutes/index.cfm?App_mode=Display_Statute&URL=0300-0399/0316/Sections/0316.6135.html
Gauer, R., and B. K. Meyers. 2019. “Heat-Related Illnesses.” American Family Physician 99(8): 482–489.
Petkova, E. P., J. K. Vink, R. M. Horton, A. Gasparrini, D. A. Bader, J. D. Francis, and P. L. Kinney. 2017. “Towards More Comprehensive Projections of Urban Heat-Related Mortality: Estimates for New York City under Multiple Population, Adaptation, and Climate Scenarios.” Environmental Health Perspectives 125(1): 47–55.
U.S. Census. 2019. “QuickFacts: Florida.” Accessed on May 18, 2021. https://www.census.gov/quickfacts/FL#qf-headnote-b
Vaidyanathan, A., J. Malilay, P. Schramm, and S. Saha. 2020. “Heat-Related Deaths—United States, 2004–2018.” Morbidity and Mortality Weekly Report 69(24): 729.
Weinberger, K. R., D. Harris, K. R. Spangler, A. Zanobetti, and G. A. Wellenius. 2020. “Estimating the Number of Excess Deaths Attributable to Heat in 297 United States Counties.” Environmental Epidemiology 4(3).
WHO. 2019. “ICD-10 Version:2019.” Accessed on May 18, 2021. https://icd.who.int/browse10/2019/en#/X30