Malaria in humans is a disease transmitted by mosquitoes in the genus Anopheles and caused by any one of four species of microscopic protozoan parasites in the genus Plasmodium (P. vivax, P. falciparum, P. malariae, and P. ovale) distributed throughout the world. Malaria was one of the major endemic diseases in the United States for more than four centuries (Russell 1968). As recently as 1935, malaria caused 4,000 deaths every year in the United States. However, by the 1940s, the annual death toll had been reduced to 400, and by 1952 it was down to 25 with little or no local transmission. In the United States and elsewhere, malaria was eradicated by draining larval habitats, treating patients with antimalarial drugs, applying mosquito larvicides and adulticides, and screening doors and windows.
Symptoms of Malaria
Symptoms of malaria vary depending on the species of malaria, but the initial attack may start with exhaustion, headache, anorexia, and occasional nausea and vomiting. The fever comprises a cold stage (shivering and a feeling of intense cold), a hot stage (distressing heat, dryness, burning, intense headache, nausea, and vomiting), and finally a profuse sweating stage. The typical attack often begins in the early afternoon and lasts from eight to twelve hours. Persons experiencing these symptoms and having been in an area with malaria should see a doctor immediately.
Clinically, malaria infections vary from moderately severe to fatal illness, depending on the species of parasite, the individual's health condition, and how soon the patient receives treatment. Malaria caused by P. falciparum is particularly severe and often fatal in infants and young children; P. vivax generally is less severe and has a lower mortality rate. Persons may be infected over and over again, usually developing a tolerance for the parasite, which prevents severe illness from reoccurring.
If insufficiently treated, a malaria infection may persist in a person for many months or years and have a continuing or periodically renewed ability to infect mosquitoes, often in the absence of symptoms or with a less-severe illness. Plasmodium vivax and P. ovale parasites may persist in the liver cells for years and give rise to relapses of the disease by reinvading the red blood cells during times of stress.
How Malaria Is Transmitted by Mosquitoes
The malaria parasite is transmitted from person to person by the bite of Anopheles mosquitoes, and ONLY Anopheles mosquitoes (Figure 2). The malaria parasite inhabits the human red blood cells, where it multiplies asexually. After reaching maturity in 48 to 72 hours, the red blood cells burst and release large numbers of new parasites, most of which enter new red blood cells, thus reinitiating the cycle. Others enter liver cells. Before the asexual cycle in red cells is established, the parasite must complete a five-to-10-day period of multiplication in liver cells. The typical malaria symptoms, chills and fever, are associated with this rupturing of infected red blood cells.
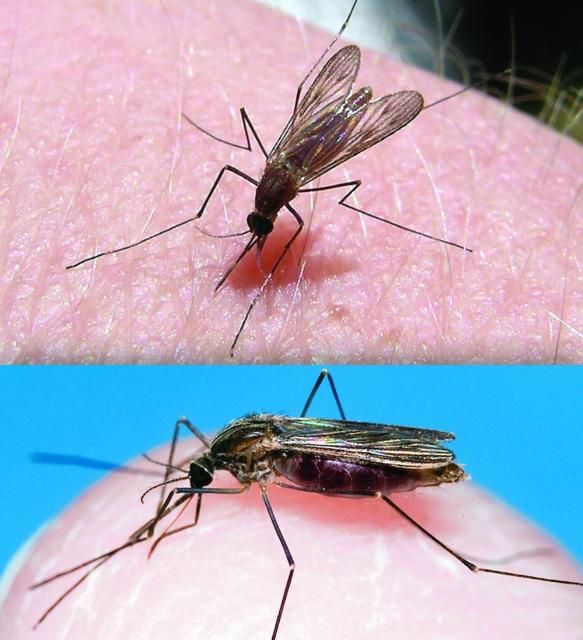
Some of the malaria parasites develop into sexual forms: the male and female gametocytes. Infection of the mosquito takes place when an Anopheles female feeds on an infected person who is carrying gametocytes. The parasite then undergoes a sexual cycle in the mosquito for the next seven to 20 days. Numerous microscopic, spindle-shaped forms, known as sporozoites, then invade the mosquito salivary glands. The human infection is initiated when sporozoites are released during the bite of the infected mosquito.
Florida's Anopheles Mosquitoes
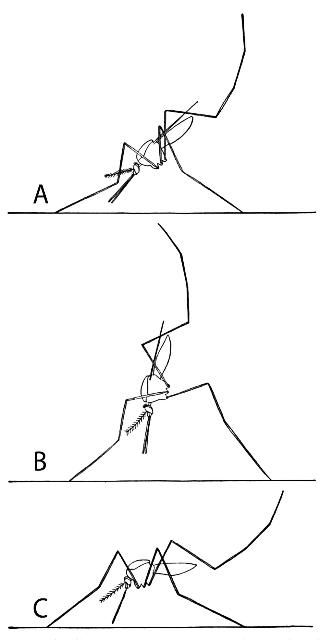
Worldwide, there are approximately 400 described species of Anopheles, but only 30 of them are of major importance in malaria transmission. Of the 75-plus species of mosquitoes occurring in Florida, 14 are in the genus Anopheles. It is easy to recognize adult Anopheles by the way they rest on a flat surface, like the skin. Unlike mosquitoes of other genera, Anopheles rest with their heads pointed downward and their bodies slanted at a steep angle upward (Figure 3). Other mosquitoes hold their bodies parallel to the resting surface. Anopheles adults also have three long mouthparts protruding from the head; other mosquitoes have one long and two short mouthparts. The immature stages of Anopheles are not easily recognized in the water, as the larvae lie near the surface and are easily confused with floating debris.
Anopheles quadrimaculatus is considered to be the most important malaria vector in Florida. Anopheles quadrimaculatus is a species complex consisting of 5 morphologically similar species (Reinert et al. 1997). The adults are dark with four spots on each wing. The larval stage is typically found in permanent bodies of fresh water containing emergent or floating vegetation. The eggs are laid singly on the water surface. During cold periods, adult females hibernate in protected sites. They feed primarily on large mammals, including humans, mostly at dusk and during the night.
Malaria in Florida in the 21st Century?
A few years ago, one may have expected that malaria would never be a problem again in the United States. However, there are and will continue to be occasional small outbreaks within the United States, including Florida. Each year over seven million US business people and tourists travel to areas where malaria is present. Also on the rise is the number of visitors to the United States from malarious areas.
In 1990, the first Florida case of human malaria (P. vivax) in 42 years was acquired, presumably through the bite of a mosquito in Gulf County. The woman who came down with malaria had no history of foreign travel, blood transfusion, or IV use. She had spent the nights of May 19 and 27, 1990, sleeping outdoors at a fish camp at Willis Landing, Gulf County. The mosquito biting activity at night was reportedly intense. No secondary cases were reported. In 1996, two residents of Palm Beach County contracted malaria, and in the same county in 2003, there were eight reported cases of locally acquired malaria. These patients had never lived in or visited a malarious area.
Economic downturns increase poverty, resulting in more people sleeping in temporary, makeshift shelters, abandoned buildings, outdoors under bridges and overpasses, or in large culverts. These same sites, while providing some protection to the homeless, are also excellent resting sites for adult Anopheles mosquitoes. Thus, now and probably for the first time since the depression years of the '30s, a larger segment of our population, including legal and illegal visitors with imported malaria, have an opportunity for increased contact with Anopheline mosquitoes, which prefer to blood feed during sunset and evening hours.
Prevention of Malaria Outbreaks in Florida
Florida's state health and related agencies should:
- Remind physicians and public health workers annually about the importation of malaria among travelers and visitors and the danger of not clinically distinguishing malaria from the more common febrile illnesses;
- Inform county health officers and mosquito control directors of imported malaria cases.
Mosquito control agencies should:
- Identify the locations of all actual and potential Anopheline larval sites;
- Survey all larval habitats annually during the peak season for Anopheles activity (June through early September);
- Identify and record the seasonal abundance of Anopheles in the county using landing rate and trap collections;
- Be informed of all imported and introduced malaria cases in the county and Florida.
Any malaria case that is not readily explained by foreign travel, visitors, or induced artificially is strongly suggestive of possible local transmission. When one case of malaria has been verified, the local public should be warned to report immediately any fever to their physician or county public health unit.
In the unlikely event of a major outbreak of malaria, the application of appropriate larvicides at known Anopheles larval sites and adulticides at resting sites is warranted to reduce the human–Anopheles contact. In addition, primary efforts should continually be made to reduce the opportunity for Anopheles to take a human blood meal by educating the public on the use of protective clothing, screens on windows and doors, repellents, and fans to keep mosquitoes away.
To avoid the risk of malaria, it is critical to avoid mosquito bites. Humans cannot get malaria from wild animals, domestic animals, or pets. Transmission of malaria from human to human is accomplished by Anopheles mosquitoes or by reuse of needles contaminated with the blood of an infected person.
Avoid mosquito bites by staying out of mosquito-infested areas, securing window screens, and by applying a repellent that has been proven to be effective. Repellents containing DEET (N,N-diethyl-3-methylbenzamide) are effective and should be used only according to the label directions.
References
Reinert, J. F., P. E. Kaiser, and J. E. Seawright. 1997. "Analysis of Anopheles (Anopheles) quadrimaculatus complex of sibling species (Diptera: Culicidae) using morphological, cytological, molecular, genetic, biochemical and ecological techniques in an integrated approach." J. Am. Mosq. Control Assoc. 13(Suppl.): 1–102.
Russell, P. F. 1968. "The United States and Malaria: Debits and Credits." Bull. N. Y. Acad. Med. 44:623.