Introduction and History
Rabbit hemorrhagic disease virus, or RHDV, is a member of the Lagovirus genus, in the virus family Caliciviridae. This virus is composed of single-stranded RNA, and does not have an envelope, or outer wrapping. Rabbit hemorrhagic disease virus infects lagomorphs, members of the taxonomic order Lagomorpha. These are mammals such as rabbits, hares, and pika (Figure 1).
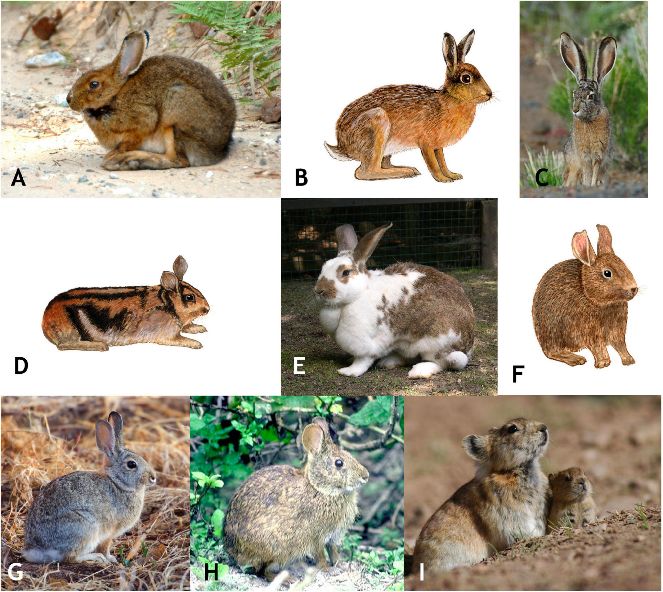
Credit: Myers et al. (2020)
Rabbit hemorrhagic disease was first discovered in 1984. The disease was detected a few days after Angora rabbits were exported from Germany to China. Over the next several months, the disease spread over 50,000 square kilometers and killed over 500,000 captive rabbits before spreading to Korea. The first reports in Europe came from Italy in October of 1986 and involved domesticated rabbits. The origin of the outbreaks in Italy is unknown. By 1988, RHDV had spread across most continents, occurring first in domesticated rabbits, and spreading later to wild rabbits. The first domesticated outbreaks of RHDV in England occurred in 1992, and reports of infections in wild rabbits began in 1994. By 1996, the disease had spread to both domesticated and wild populations throughout Britain and Ireland.
There are a few possible sources of RHDV: mutation from a European brown hare syndrome virus (EBHS), mutation from a preexisting nonpathogenic lagomorph virus, or transfer of an unknown virus from another animal species. The second possibility is most likely, indicated by serum proteins reacting with antigen-antibody complexes. Despite these three theories, scientists are still trying to better understand the distribution, patterns, and outbreaks of RHDV.
A new strain of RHDV, known as RHDV2, was identified in France in 2010. This new virus had a capsid protein sequence with 80% similarity to RHDV, meaning the protein shell that protects the viral genome of each virus was very similar. Rabbit hemorrhagic disease virus serotype 2 can cause disease in both vaccinated and young, susceptible rabbits. The virus spread throughout Europe and, as a result, mortality rates and cases of acute RHD began to increase. Two Italian strains of RHDV2 found and isolated in 2014 and 2015 had mortality rates of over 80%, which is similar to that of RHDV. Rabbit hemorrhagic disease virus-2 has been present throughout Europe since 2011. It is evolving and spreading rapidly.
The first report of RHDV2 in the United States involved a domesticated rabbit in Ohio in 2018. Since this first detection of the virus, RHDV2 has spread throughout the country and has been found in both wild and domesticated rabbits (Figure 2). The New Mexico Department of Game and Fish has confirmed RHDV2 in wild black-tailed jackrabbit and desert cottontail populations. Texas and Arizona have also confirmed wild rabbit deaths due to RHDV2. Thus far, no endangered rabbit species in the United States have been impacted by RHDV2. The first report of the virus in Florida came from a domesticated rabbit in Lake County on December 30, 2020. The second and most recent report of the virus in Florida was from yet another domesticated rabbit in St. Johns County on October 18, 2021. It is unknown how the virus spread to Florida; however, there have not been any reported cases of the virus in wild rabbits in the state.
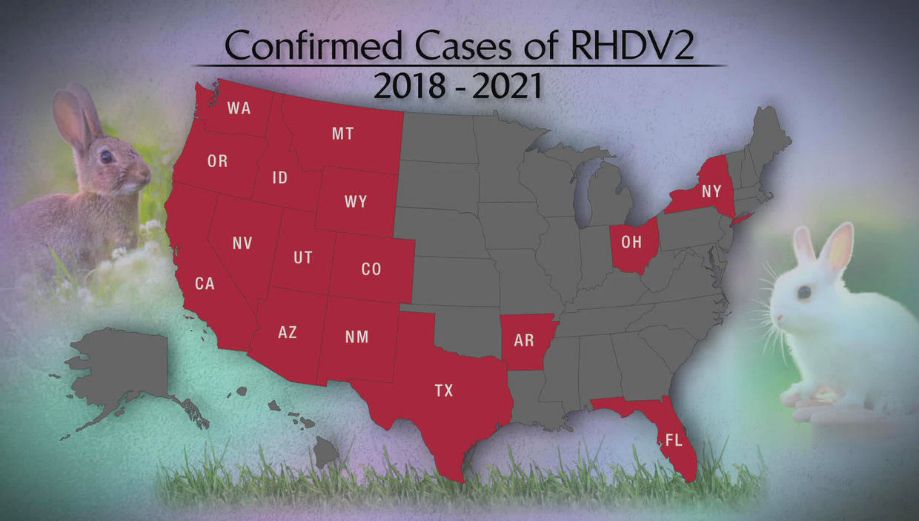
Credit: Wildlife Health.org
Infection
Rabbit hemorrhagic disease virus-2 is resistant to extreme temperatures and highly contagious. It can spread through direct contact with an infected rabbit or exposure to its blood, urine, feces, and other excretions. The virus can also survive in and spread from carcasses of infected rabbits, contaminated food and water sources, and enclosures where infected rabbits were kept if not properly decontaminated. It can be contracted through oral, respiratory, and conjunctival routes as well as through wounds or trauma on the skin. Humans can indirectly spread the virus by carrying it on their clothing and shoes.
The virus can survive in a decaying carcass for several weeks. A study reported by the Texas Animal Health Commission showed a viable virus in a carcass after 90 days of being exposed to the environment. The incubation period, or the time from first exposure to the first clinical sign of RHDV2, ranges from 3–9 days. Once clinical signs are apparent, death can occur in 1–3 days. Rabbits of any age can contract RHDV2. If you suspect your rabbit has contracted the virus, consult your veterinarian for guidance.
Clinical Signs
The first and most common clinical sign of the virus is sudden, unexpected death of rabbits, regardless of quality of health. Rabbits who do not die will likely have poor appetite and exhibit malaise, depression, and overall disinterest. Fever and bloody nasal discharge are common. Other clinical signs include organ failure, jaundice, respiratory issues, diarrhea, weight loss, and bloating. Rabbits who survive continue to shed the virus, or release the virus into the environment, for 30 to over 100 days. Rabbits who survive the virus do have immunity, but the duration of immunity is unknown. Note that humans are not at risk of contracting this virus.
Treatment
There is no cure for RHDV2, only supportive care to help the animal through the infection. Preventive treatment is available through a few vaccines to protect against RHDV2, with other vaccines available for protection against RHDV. The first two available vaccines are killed virus vaccines licensed in the European Union (EU). These may be used in the United States with special authorization. A third US-based killed virus vaccine is distributed from Medgene Labs and prevents shedding of the virus or spreading of infection once given to a rabbit.
Prevention
It is important to practice biosecurity to prevent the spread and/or introduction of a virus. Several methods can limit the spread of the virus as well as protect your rabbits from becoming infected.
- Do not allow wild rabbits to have contact with your domesticated rabbits or to gain entry to the space where you keep your domestic rabbits.
- Guests should wash their hands with warm water and soap for at least 20 seconds before coming in contact with your domestic rabbits. Guests with pet rabbits should not have access to your rabbit area, as the virus can be indirectly transmitted from clothing and shoes.
- Always wash hands with warm water and soap for at least 20 seconds before entering your rabbit area, after removing protective clothing (coveralls, shoe coverings, gloves, hair coverings), and before leaving the rabbit area.
- If you wish to introduce new rabbits into your rabbit area, keep them separated from your current rabbits for at least 30 days. Use separate equipment for newly acquired or sick rabbits to avoid spreading disease.
- Sanitize all equipment and cages with 10% bleach or 10% sodium hydroxide mixed with water before and after new rabbits are introduced.
- Consult a veterinarian on proper biosecurity practices and if any of your rabbits appears sick or is found dead.
- If you live near or visit an area where RHDV2 has been detected, do not interact with or remove any dead wild rabbits you may see. Instead, contact state/federal wildlife officials and inform them of your findings.
- If you find multiple dead wild rabbits, contact state/federal wildlife officials.
- Never release domesticated rabbits into the wild.
- Before disposing of a rabbit that has died, consult your veterinarian, or contact state/federal wildlife officials for guidance.
Reporting
If you find a sick or dead wild rabbit, report your findings to the Florida Fish and Wildlife Conservation Commission at (850) 488-4676, call the Wildlife Health Hotline at (866) 293-9282, or email FWC at wildlifehealth@myFWC.com. If any of your domesticated rabbits becomes sick or dies, report to the Division of Animal Industry at RAD@FDACS.gov or call (850) 410-0900. All rabbits imported into Florida from a non-RHDV-affected state must have an Official Certificate of Veterinary Inspection (OCVI) within 30 days of entry. All rabbits imported into Florida from an RHDV-affected state must have an OCVI within 72 hours of entry as well as a veterinary statement. Reporting any clinical signs in domesticated rabbits to prevent spread of the virus to wild rabbits is important. Currently, there have been no reports of wild rabbits contracting RHDV2 in Florida; only domestic cases have been reported.
References
Capucci, L., P. Cavadini, M. Schiavitto, G. Lombardi, and A. Lavazza. 2017. “Increased Pathogenicity in Rabbit Hemorrhagic Disease Virus Type 2 (RHDV2).” Veterinary Record 180(17): 426. https://doi.org/10.1136/vr.104132
Duff, J. P. 2012. “Calicivirus Infections.” In Infectious Diseases of Wild Mammals and Birds in Europe, edited by A. Meredith, Widén Dolores Gavier, and J. P. Duff. 73–80. Wiley-Blackwell.
Florida Department of Agriculture and Consumer Services. 2021. “Rabbit Hemorrhagic Disease Update.” Tallahassee, Florida: Division of Animal Agriculture. Accessed December 9, 2021. https://www.fdacs.gov/content/download/98220/file/RHD2-Website-20211019.pdf
Medgene Labs. 2021. “Medgene Labs Receives Emergency Use Authorization for RHDV2 Vaccine.” Retrieved December 9, 2021. https://medgenelabs.com/rhdv2-vaccine/
Myers, P., R. Espinosa, C. S. Parr, T. Jones, G. S. Hammond, and T. A. Dewey. 2020. “The Animal Diversity Web.” Accessed December 9, 2021. https://animaldiversity.org
Sleeman, J. 2020. “Rabbit Hemorrhagic Disease Virus 2 Confirmed in Wild Rabbits in the United States.” USGS National Wildlife Health Center.
Texas Animal Health Commission. 2020. “Rabbit Hemorrhagic Disease FAQ.” Austin.
United States Department of Agriculture. 2020. “Rabbit Hemorrhagic Disease Fact Sheet.” Fort Collins.
Wildlife Health.org. 2022. “Rabbit Hemorrhagic Disease Virus 2 in the U.S.: Current Updates – March 2022. Current Disease Event Information: Updated March, 2022.” Accessed March 16, 2022. https://wildlifehealth.org/rabbit-hemorrhagic-disease-virus/