What is swimmer's itch?
Swimmer's itch, also known as cercarial dermatitis, is a skin rash caused by infection with parasitic flatworms in the family Schistosomatidae, also known as schistosomes. People develop swimmer's itch only after bathing in water containing the parasites. Humans are noncompatible, accidental hosts and are infected when the larval worms penetrate their skin while looking for a compatible wildlife host, like a bird, dog, raccoon, rodent, or other animal. In the United States, the schistosomes most likely to cause swimmers itch are those that infect birds and dogs as their hosts. In other countries, schistosomes that use humans as their main host cause a disease known as schistosomiasis (in this article that disease is not covered). Although the rash is uncomfortable, the worms that cause swimmer's itch cannot mature into adult worms or cause disease in humans.
What causes swimmer's itch?
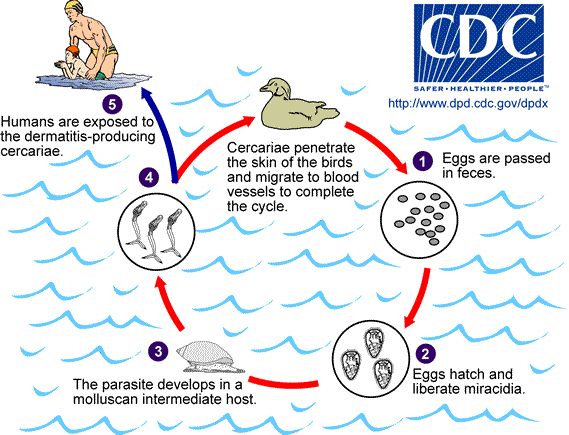
There are several different species of schistosomes that can cause swimmer's itch in people in the United States. They all normally parasitize (infect) animals other than humans, especially dogs and waterfowl, like ducks and geese. The parasite's life cycle includes a stage in an aquatic snail species (Figure 1). The snail is infected by a free-swimming stage of the parasite known as a miracidium (stage 2 in Figure 1). The method of penetration depends upon the schistosome species, and penetration may occur through multiple methods within the same species. These penetration methods include ingestion of eggs or miracidia, direct penetration of the snail tegument (skin), and entry through natural openings. Next, inside the snail, the parasite replicates and then leaves the snail as another free-swimming stage, the cercaria. These cercariae (stage 4 in Figure 1) search for a vertebrate host to complete the next stage of the life cycle. Cercariae can sense shadows, water turbulence, temperature, and body odor that reveal the presence of a host. They penetrate the skin, usually of the foot or leg, and once inside the vertebrate host, the worms mature, mate, and migrate through the circulatory system to the veins surrounding the gut, where they lay eggs. The eggs make their way into the gut, where they are expelled when the host defecates into the water. In the water, the miracidia hatch from the eggs, and the life cycle continues. The parasite may be present wherever its snail and vertebrate hosts are present in fresh or brackish water.
Credit: Centers for Disease Control and Prevention (CDC)
Why do humans get infected?
When the cercariae (Figure 2) are searching for a host to complete their life cycle, occasionally they infect an unsuspecting person swimming or wading in the water. Humans are not the preferred host of the parasitic worms, and infections in people are incidental. The cercariae penetrate the skin of the human but soon die because the parasitic worm cannot mature in the human host. Unfortunately, this is not the end of the problem, because our immune systems attack these foreign bodies, causing an inflammatory reaction that can be very itchy and uncomfortable. This inflammatory reaction is what we call swimmer's itch.

How do you know if you have swimmer's itch?
When you dry off, the skin may tingle, and the rash will appear shortly after swimming (within 12 hours). The red spots (macules) will get redder and become itchier as time progresses before eventually subsiding (Figure 3). Each red spot is the site where a single cercaria (immature worm) penetrated the skin. A small papule (solid raised spot with no fluid) will appear at each penetration site within 10 to 15 hours. Vesicles (fluid-filled areas 1–2 mm in diameter) will develop on these papules within 2 to 3 days. The degree of discomfort varies between individuals, with repeated exposures usually resulting in more intense reactions. Swimmer's itch can be mistaken for a poison ivy reaction. However, the rash due to swimmer’s itch causing parasitic flatworms results in small raised papules, whereas that caused by poison ivy usually results in larger, fluid-filled blisters. Chigger bites and seabather's eruption (caused by small jellyfish) may also be confused with swimmer's itch. However, in both of those cases, the bites or stings from the organisms will be mainly around the edges of clothing. In swimmer's itch, the papules are usually on areas of exposed skin and not on areas of skin that were covered by tight-fitting garments. Swimmer's itch, therefore, is usually found on the arms or legs or other areas not protected by a bathing suit or other clothing. As pictured in Figure 3, the lower legs and arms from elbow to wrist were covered with papules, however the reaction was not found on other parts of the body.

Credit: Emma N. I. Weeks, UF/IFAS
How can people avoid swimmer's itch?
Swimmer's itch is fairly uncommon because the parasites prefer to infect other species instead of humans. For a swim in a body of water to result in swimmer's itch, the correct invertebrate (snail) and vertebrate (e.g., duck or dog) host species must have been present.
Symptoms in infected dogs can be severe, including lethargy, weight loss, vomiting, and diarrhea. Untreated infected dogs may die of liver and/or renal failure. Undiagnosed dogs may continue to contribute to the infection of other hosts, including humans. If your dog appears to be unwell and has been exposed to snail habitats (water bodies with abundant vegetation) consult a veterinarian.
Even if all the right species are present, the number of cercariae present may not be enough to cause swimmer's itch. However, if the lake has abundant snails (usually associated with aquatic plants such as hydrilla) and many aquatic birds or dog activity, then the probability that swimmers in the lake will contract swimmer's itch will increase (see Figure 4 for an example of the appropriate habitat). In warmer water, where these other hosts (ducks and snails) are abundant, your risk may be increased. In this situation, the following steps can minimize the risk of a swimmer's itch problem:
- Do not swim in shallow water for long periods of time. Snails are present in shallow water, and birds and dogs wade there, so these areas may have especially high concentrations of cercariae.
- Avoid swimming in lakes where dogs are permitted to access the water and could defecate in the water or on the shoreline.
- Rinse and dry off immediately after getting out of the water rather than "air drying." Some worm species penetrate the skin as the water dries on the body.
- Avoid swimming on sunny warm days, especially in the mornings. Laboratory-based studies showed that cercariae were released most rapidly from snails at these times.
- If you do develop a rash after swimming and you are concerned, consult your physician.

Credit: Emma N. I. Weeks, UF/IFAS
References
Al-Jubury, A., Y. Duan, P. Kania, E. Tracz, A. Bygum, L.v.G. Jørgensen, P. Horák, and K. Buchmann. 2021. “Avian schistosome species in Danish freshwater lakes: Relation to biotic and abiotic factors.” Journal of Helminthology 95: E22. https://doi.org/10.1017/S0022149X21000122
Centers for Disease Control and Prevention. "Parasites - Cercarial dermatitis (also known as Swimmer's itch)." https://www.cdc.gov/parasites/swimmersitch/index.html (15 December 2021).
Kolárová L., P. Horák, K. Skírnisson, H. Marecková, and H. Doenhoff. 2013. "Cercarial dermatitis, a neglected allergic disease." Clinical Reviews in Allergy and Immunology 45: 63–74. https://doi.org/10.1007/s12016-012-8334-y
Rodriguez, J. Y., B. C. Lewis, and K. F. Snowden. 2014. "Distribution and characterization of Heterobilharzia americana in dogs in Texas." Veterinary Parasitology 102: 35–42. https://doi.org/10.1016/j.vetpar.2014.03.026
Sckrabulis, J., A. Flory, and T. Raffel, T. 2020. Direct onshore wind predicts daily swimmer's itch (avian schistosome) incidence at a Michigan beach. Parasitology 147: 431-440. https://doi.org/10.1017/S0031182020000074
Verbrugge, L., J. J. Rainey, R. L. Remimink, and H. D. Blankespoor. 2004. "Swimmer's itch: Incidence and risk factors." American Journal of Public Health. 94: 738–741. https://doi.org/10.2105/AJPH.94.5.738