The genus Rickettsia contains species that are important in human health as they cause several serious diseases such as Rocky Mountain spotted fever. This publication summarizes the human-disease-causing pathogens in the genus Rickettsia in the United States and delivers general knowledge of their vectors and the diseases they cause. Prevention and management of disease-causing Rickettsia species, mainly for vector control agencies and entities, are also discussed. This publication is written for audiences of all ages and with any educational background and serves as a resource for public education.
Introduction
Rickettsia is a bacterial genus in the Order Rickettsiales and Family Rickettsiaceae. Rickettsia are intracellular bacteria, meaning that they must reside within host cells to survive and cannot be cultured artificially. The Rickettsia genus contains species that are well-known as causative agents of diseases (pathogens) in humans and other mammals such as Rocky Mountain spotted fever (RMSF) and epidemic typhus. Epidemic typhus has caused millions of deaths in human history. Based on serological characteristics, Rickettsia was originally classified into three groups: spotted fever group, typhus group, and scrub typhus group. In 1995, the causative agent of the scrub typhus group, formerly Rickettsia tsutsugamushi, was reclassified to the genus Orientia and is now known as Orientia tsutsugamushi based on phenotypic and genotypic differences (Tamura et al. 1995), leaving two groups classified in Rickettsia. Vector-borne species within the genus Rickettsia are transmitted by a wide range of vectors, including ticks, fleas, mites, and lice. Some Rickettsia species, such as Rickettsia rickettsii, can be transmitted biologically through transstadial transmission (from one vector life stage to the next, i.e., larva to nymph and nymph to adult) and transovarial transmission (from female to offspring). It should be noted that most recognized Rickettsia are not known to cause disease in mammals. Many Rickettsia species are non-pathogenic endosymbionts (organisms that live within the body of another organism without harming the host) of ticks (Bonnet et al. 2017).
Human Disease-Causing Rickettsia in the United States
According to the Centers for Disease Control and Prevention (CDC), there are four species of Rickettsia from the spotted fever group and two species from the typhus group that occur in the United States. Those in the spotted fever group are Rickettsia rickettsii, the agent of Rocky Mountain spotted fever; Rickettsia parkeri, the agent of Rickettsia parkeri rickettsiosis; Rickettsia philipii, the agent of Pacific Coast tick fever; and Rickettsia akari, the agent of rickettsialpox. The typhus group contains Rickettsia typhi, the agent of murine typhus; and Rickettsia prowazekii, the agent of epidemic typhus. The treatment of Rickettsia-caused disease usually involves antibiotics. In the United States, the most serious and commonly reported disease is RMSF. Other Rickettsia-caused diseases are uncommon or rare.
People may be exposed to other disease-causing Rickettsia species during travel outside of the United States and thus these infections are reported as imported spotted fevers. The most commonly imported spotted fevers are African tick bite fever caused by Rickettsia africae and Mediterranean spotted fever caused by Rickettsia conorii. Common symptoms of spotted fevers are similar to each other and include fever, headache, and rash. Rickettsia species can be difficult to diagnose based only on clinical symptoms and require a laboratory test for confirmation.
Humans acquire Rickettsia pathogens primarily through bites or fecal introduction from infected arthropod vectors. Within the spotted fever group, Rickettsia rickettsii is primarily transmitted by the American dog tick, Dermacentor variabilis Say, in the eastern United States; the Rocky Mountain wood tick, Dermacentor andersoni Stiles, in the Rocky Mountain region and western Canada; or the brown dog tick, Rhipicephalus sanguineus (Latreille), in Mexico and Arizona in the United States (Dantas-Torres 2007). The primary vectors of Rickettsia parkeri, Rickettsia philipii, and Rickettsia akari are the Gulf Coast tick, Amblyomma maculatum Koch; the Pacific Coast tick, Dermacentor occidentalis Marx; and mouse mites, Liponyssoides sanguineus (Hirst), respectively (CDC 2019). Within the typhus group, Rickettsia typhi and Rickettsia prowazekii are primarily transmitted by fleas and human body lice, respectively (CDC 2020a, b). All but one of these six species can be transmitted both transstadially and transovarially. The single exception is Rickettsia prowazekii, which can only be transmitted transstadially (Azad and Beard 1998).
Spotted Fever Group Rickettsia
Rickettsia rickettsii
Rickettsia rickettsii is an intracellular bacterium and is the agent that causes RMSF. The primary vectors of Rickettsia rickettsii are the American dog tick (Figure 1a) in the United States, the Rocky Mountain wood tick (Figure 1b) in Canada, the brown dog tick in Mexico, and the Cayenne tick (Amblyomma cajennense Fabricius) (Figure 1c) in Central and South America (Dantas-Torres 2007). Hard ticks also serve as natural reservoirs (the organisms in which pathogens naturally live and reproduce) by transstadial and transovarial transmission. When infected ticks attach and feed on humans, Rickettsia rickettsii are released from tick salivary glands and transferred to humans, a process that may take 6–10 hours on average and 24 hours or longer in some cases (Thorner et al. 1998). Humans usually acquire Rickettsia rickettsii from bites of infected ticks, although it is possible to acquire infection by contacting tick tissue and fluids during tick removal (Walker and Raoult 1995) and through blood transfusion (Wells et al. 1978).
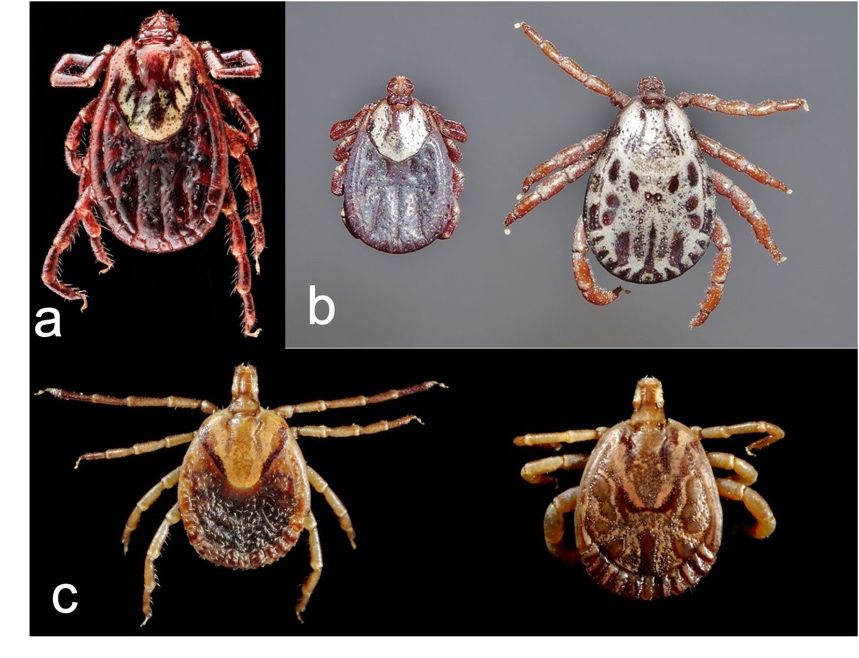
Credit: a) Sam Droege Wikimedia Commons, https://creativecommons.org/licenses/by/4.0/deed.en; b) Daktaridudu, Wikimedia Commons, https://creativecommons.org/licenses/by/4.0/deed.en; c) Centers for Disease Control and Prevention
Patients develop symptoms after an approximate 7-day incubation period (the period between exposure to a pathogen and the first appearance of symptoms). The common symptoms of RMSF are not specific but include headache, fever, rash, nausea, and vomiting. However, a characteristic maculopapular rash (a rash that has both flat discolored areas and small raised bumps) typically occurs 2–5 days after fever onset in most patients. The rash first appears on the hands and feet and gradually spreads to cover the entire body. This progression pattern of the rash is an important clinical feature that can assist in distinguishing it from rashes produced by other vector-borne pathogens (Nicholson et al. 2009). Diagnosis of RMSF is difficult due to the unspecific symptoms and difficulties in differentiating between bacteria species in the spotted fever group. Treatment of RMSF often involves antibiotics, and early treatment is critical to prevent death and severe illness from RMSF (CDC 2022).
RMSF occurs mainly in countries of the Western Hemisphere and is distributed widely in the United States. Beginning in January 2010, RMSF cases have been reported in a new category called spotted fever rickettsiosis due to the difficulties in differentiating Rickettsia rickettsii from other species in the spotted fever group using commonly available serologic tests (A serologic test checks the substances in a blood sample) (CDC 2022). In 2018 and 2019, the total reported case numbers of spotted fever rickettsiosis were 5,544 and 5,207 in the United States, respectively.
Other Spotted Fever Rickettsia
Rickettsia parkeri, Rickettsia philipii (known previously as Rickettsia species 364D), and Rickettsia akari are the three other spotted fever group Rickettsia species known to occur in the United States that can cause diseases: Rickettsia parkeri rickettsiosis, Pacific Coast tick fever, and rickettsialpox, respectively (CDC 2019). The primary vector of Rickettsia parkeri is the Gulf Coast tick (Amblyomma maculatum) (Figure 2a), which is distributed in the southeastern and southcentral United States. The Pacific Coast tick (Dermacentor occidentalis) (Figure 2b) is the primary vector of Rickettsia philipii, and this tick is found along the Pacific Coast in California, Oregon, and Washington. Unlike Rickettsia parkeri and Rickettsia philipii, which are transmitted by ticks, Rickettsia akari is transmitted by mouse mites (Liponyssoides sanguineus), which are often reported in the northeastern United States (CDC 2019). These spotted fevers typically are less severe than RMSF.

Credit: a) Centers for Disease Control and Prevention; b) Jerry Kirkhart, Wikimedia Commons, https://creativecommons.org/licenses/by/4.0/deed.en
The first sign of these spotted fevers is an eschar (a dark scab) at the tick bite site. Generally, an eschar does not occur with RMSF, and it is used as a clinical sign to differentiate the less severe spotted fevers from RMSF (Drexler et al. 2020). Other symptoms, such as fever, headache, rash, and muscle aches may occur several days after the appearance of an eschar. Diagnosis of spotted fevers can be difficult due to non-specific symptoms in the early stage and the fact that laboratory tests can return a false negative in the first 7–10 days of illness. Tick or mite exposure and clinical evidence are helpful for diagnosis.
Typhus Group
Rickettsia typhi
Rickettsia typhi is an agent that causes murine typhus, also called flea-borne typhus and endemic typhus. Murine typhus is found throughout the world. In the United States, murine typhus is endemic (regularly occurring within a certain area) in parts of California, Hawaii, and Texas with more than 100 reported cases per year. Rickettsia typhi is an obligate intracellular bacterium and is transmitted by infected flea feces. Scratching a flea bite wound can rub rickesttsiae contained in flea feces into the wound and cause infection. It is also possible to acquire the bacteria by inhaling infected flea feces or rubbing it into the eyes (CDC 2020a). Rickettsia typhi usually is maintained in a rodent–flea cycle (Adjemian et al. 2010). Natural infection has been detected in at least 11 flea species including the cat flea (Ctenocephalides felis) (Figure 3). The primary reservoirs are black rats (Rattus rattus) and Norway rats (Rattus norvegicus). Other animals, such as peridomestic rats, house mice, oldfield mice, domestic cats, and Virginia opossums, also serve as reservoirs (Blanton et al. 2022). Infection in rats is persistent but not fatal, which enables rats to serve as an infection source.

Credit: Katja ZSM, Wikimedia Commons, https://creativecommons.org/licenses/by/4.0/deed.en
Symptoms of Rickettsia typhi infection or murine typhus may occur within two weeks after infection. Common symptoms include fever, rash, muscle and joint pain, vomiting, and cough. Human fatality rates from murine typhus are usually low (<5%) without treatment (Durden and Hinkle 2019). However, untreated disease can cause damage to one or more organs (CDC 2020a). Diagnosis of murine typhus is usually performed by antibody detection and isolation of bacteria in a blood or tissue sample (Durden and Hinkle 2019).
Rickettsia prowazekii
Rickettsia prowazekii is the agent that causes epidemic typhus, also known as louse-borne typhus, or louse-borne fever. Epidemic typhus is rare in the United States and often occurs in areas of widespread body louse infestations, overcrowding, and poor sanitary conditions (Durden 2019). Rickettsia prowazekii is transmitted by the human body louse (Pediculus humanus humanus Linnaeus) (Figure 4) via louse feces. Human body lice become infected during blood feeding on infected people with Rickettsia prowazekii circulating in their bloodstreams. Infective rickettsiae invade and multiply in louse gut cells without invading other tissues, which results in the posterior station (transmission via infected louse feces) and transstadial transmissions only (Durden 2019). Susceptible humans become infected with the rickettsiae when louse feces are rubbed into louse bite wounds. Lice infected with Rickettsia prowazekii die within one week as infection causes their gut cells to rupture (Houhamdi et al. 2002). Rickettsia prowazekii can remain viable in louse feces for up to 100 days (Raoult and Roux 1999). Humans and human body lice serve as primary reservoirs of Rickettsia prowazekii, although it has been detected in other animals, such as flying squirrels and ticks (Reynolds et al. 2003; Medina-Sancheza et al. 2005).

Credit: Centers for Disease Control and Prevention
Symptoms of Rickettsia prowazekii infection occur within two weeks after infection and include fever, headache, malaise, and cough. Within 4–7 days after initial symptoms, a rash usually occurs and spreads from the abdomen to the chest and then, often, to most of the rest of the body (Durden 2019). Fatality of epidemic typhus was estimated at up to 60% without treatment and decreased to approximately 4% with appropriate treatment (Bechah et al. 2008). Patients who recovered from epidemic typhus without treatment sometimes maintained Rickettsia prowazekii undetected in their bodies for months or years (Price et al. 1958; McQuiston et al. 2010). A weakened immune system may increase the chances of a latent infection reactivating. The pathogen can reinvade and cause disease again, which is called recrudescent typhus or Brill-Zinsser disease. The symptoms of recrudescent typhus are similar to the initial illness but milder (CDC 2020b). Diagnosis of epidemic typhus usually involves serological tests and advanced laboratory tests (Bechah et al. 2008).
Prevention and Management
For the spotted fevers and typhus discussed above, there is no vaccine available, and the best prevention method is vector management.
Ticks have wide habitat ranges including grassy, brushy, or wooded areas, and brown dog ticks can survive indoors. Ticks may be picked up when humans or pets contact vegetation in these habitats. Thus, personal protection, such as repellents, should be considered, and tick checks should be performed after walking in tick habitat. Multiple application methods are available for treatment of livestock and companion animals with approved acaricides, including pour-on, spot-on, sprays, self-treatment stations, and ear tags. To avoid poisoning and acaricide resistance, label directions of acaricides must be followed during use. Some animal species and breeds may be sensitive to certain acaricides, so a veterinarian should be consulted as needed, and labels must always be followed. Ticks found on humans and other animals should be removed immediately using fine-tip forceps. If the tick is attached, the forceps should be used to grab it as close to the skin as possible and pull it directly away from the attachment site. For more tick information, please visit the CDC’s tick webpage, at https://www.cdc.gov/ticks/index.html.
Fleas often are found on pets and wild animals. Veterinarian-approved flea control products should be used to treat or prevent flea infestation of pets, especially for pets that are allowed outside. Rodents and other wild mammals should be kept away from living areas by removing trash and tall vegetation and sealing holes in homes. Consult with rodent control experts as needed. Flea bites can occur during contact with stray animals and when handling sick animals. Thus, gloves and other personal protection should be worn when contacting wild or sick animals. For more flea control information, please see the Ask IFAS publication, Fleas, https://edis.ifas.ufl.edu/publication/IG087.
Human body lice thrive in places that are overcrowded and where proper sanitation is not possible. Human body lice most frequently are found on clothing, where they lay their eggs. Aside from disposing of infested fabrics, washing all clothing and bedding in hot water and drying at a high temperature is one of the best methods to eliminate a body louse infestation. In the United States, flying squirrels serve as a reservoir of Rickettsia prowazekii, and, thus, people should avoid contact with flying squirrels and their nests. For more body lice treatment information, please visit the CDC’s body lice treatment page at https://www.cdc.gov/parasites/lice/body/treatment.html.
Rickettsia in Florida
Several tick species that transmit Rickettsia species in the spotted fever group are found in Florida, including the American dog tick, the brown dog tick, and the Gulf Coast tick. However, the total number of reported spotted fever cases (RMSF and other spotted fevers) was less than 32 cases every year since 2002 (FDOH 2020a). Typhus is rare in Florida, with only two reported cases of murine typhus from the past decade (FDOH 2020b).
References
Adjemian, J., S. Parks, K. McElroy, J. Campbell, M. E. Eremeeva, W. L. Nicholson, J. McQuiston, and J. Taylor. 2010. “Murine Typhus in Austin, Texas, USA, 2008.” Emerging Infectious Diseases 16:412–417. https://doi.org/10.3201/eid1603.091028
Azad, A. F., and C. B. Beard. 1998. “Rickettsial Pathogens and Their Arthropod Vectors.” Emerging Infectious Diseases 4:179–186. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2640117/
Bechah, Y., C. Capo, J. L. Mege, and D. Raoult. 2008. “Epidemic Typhus.” The Lancet Infectious Diseases 8:417–426. https://doi.org/10.1016/S1473-3099(08)70150-6
Blanton, L. S., B. R. Quade, A. Ramírez-Hernández, N. L. Mendell, A. Villasante-Tezanos, D. H. Bouyer, J. L. VandeBerg, and D. H. Walker. 2022. “Experimental Rickettsia typhi Infection in Monodelphis domestica: Implications for Opossums as an Amplifying Host in the Suburban Cycle of Murine Typhus.” The American Journal of Tropical Medicine and Hygiene.” 107:102–109. https://doi.org/10.4269/ajtmh.21-1076
Bonnet, S. I., F. Binetruy, A. M. Hernández-Jarguín, and O. Duron. 2017. “The Tick Microbiome: Why Non-Pathogenic Microorganisms Matter in Tick Biology and Pathogen Transmission.” Frontiers in Cellular and Infection Microbiology 7:236.https://doi.org/10.3389/fcimb.2017.00236
Centers for Disease Control and Prevention (CDC). 2007. Table II. (Part 6) Provisional Cases of Selected Notifiable Diseases, United States, Week Ending December 30, 2006. https://wonder.cdc.gov/nndss/nndss_weekly_tables_1995_2014.asp?mmwr_year=2006&mmwr_week=52&mmwr_table=2F&request= (accessed Jan. 12, 2023).
Centers for Disease Control and Prevention (CDC). 2019. Other Spotted Fever Group Rickettsioses. https://www.cdc.gov/otherspottedfever/transmission/index.html (accessed Jan. 12, 2023).
Centers for Disease Control and Prevention (CDC). 2020a. Flea-Borne (Murine) Typhus. https://www.cdc.gov/typhus/murine/index.html (accessed Jan. 12, 2023).
Centers for Disease Control and Prevention (CDC). 2020b. Epidemic Typhus. https://www.cdc.gov/typhus/epidemic/index.html (accessed Jan. 12, 2023).
Centers for Disease Control and Prevention (CDC). 2022. Rocky Mountain Spotted Fever. https://www.cdc.gov/rmsf/stats/index.html (accessed Jan. 12, 2023).
Dantas-Torres, F. 2007. “Rocky Mountain Spotted Fever.” The Lancet Infectious Diseases 7:724–732. https://doi.org/10.1016/S1473-3099(07)70261-X
Drexler, N., K. Nichols Heitman, and C. Cherry. 2020. “Description of Eschar-Associated Rickettsial Diseases Using Passive Surveillance Data — United States, 2010–2016.” Morbidity and Mortality Weekly Report 68:1179–1182. https://doi.org/10.15585/mmwr.mm685152a2
Durden, L. 2019. Chapter 7 — “Lice (Phthiraptera).” In Medical and Veterinary Entomology, 3rd edition, edited by G. R. Mullen and L. A. Durden, 79–106. San Diego, California: Academic Press. https://doi.org/10.1016/B978-0-12-814043-7.00007-8
Durden, L., N. C. Hinkle. 2019. Chapter 10 — “Fleas (Siphonaptera).” In Medical and Veterinary Entomology, 3rd edition, edited by G. R. Mullen and L. A. Durden, 145–169. San Diego, California: Academic Press. https://doi.org/10.1016/B978-0-12-814043-7.00010-8
Florida Department of Health (FDOH). 2020a. Rocky Mountain Spotted Fever And Spotted Fever Rickettsiosis. http://www.flhealthcharts.com/Charts/OtherIndicators/NonVitalIndNoGrpCountsDataViewer.aspx?cid=0182 (accessed Jan. 12, 2023).
Florida Department of Health (FDOH). 2020b. Typhus Fever. http://www.flhealthcharts.com/charts/OtherIndicators/NonVitalIndNoGrpCountsDataViewer.aspx?cid=0188 (accessed Jan. 12, 2023).
Houhamdi, L., P. E. Fournier, R. Fang, H. Lepidi, and D. Raoult. 2002. “An Experimental Model of Human Body Louse Infection with Rickettsia prowazekii.” Journal of Infectious Diseases 186:1639–1646. https://doi.org/10.1086/345373
McQuiston, J. H., E. B. Knights, P. J. DeMartino, S. F. Paparello, W. L. Nicholson, J. Singleton, C. M. Brown, R. F. Massung, and J. C. Urbanowski. 2010. “Brill-Zinsser Disease in a Patient following Infection with Sylvatic Epidemic Typhus Associated with Flying Squirrels.” Clinical Infectious Diseases 51:712–715. https://doi.org/10.1086/655891
Medina-Sancheza, A., D. H. Bouyer, V. Alcantara-Rodriguez, C. Mafra, J. Zavala-Castro, T. Whitworth, V. L. Popov, I. Fernandez-Salas, and D. H. Walker. 2005. “Detection of a Typhus Group Rickettsia in Amblyomma Ticks in the State of Nuevo Leon, Mexico”. Annals of the New York Academy of Sciences 1063: 327–332. https://doi.org/10.1196/annals.1355.052
Nicholson, W. L., D. E. Sonenshine, B. H. Noden, and R. N. Brown. 2019. “Ticks (Ixodida)” in Medical and Veterinary Entomology, 3rd edition, edited by G. R. Mullen and L. A. Durden, 603–672. San Diego, California. Academic Press. https://doi.org/10.1016/B978-0-12-814043-7.00027-3
Price, W. H., H. Emerson, H. Nagel, R. Blumberg, and S. Talmadge. 1958. “Ecologic Studies on the Interepidemic Survival of Louse-Borne Epidemic Typhus Fever.” American Journal of Hygiene 67:154–178. https://doi.org/10.1093/oxfordjournals.aje.a119925
Raoult, D., and V. Roux. 1999. “The Body Louse as a Vector of Reemerging Human Diseases.” Clinical Infectious Diseases 29:888–911. https://doi.org/10.1086/520454
Reynolds, M. G., J. W. Krebs, J. A. Comer, J. W. Sumner, T. C. Rushton, C. E. Lopez, W. L. Nicholson, et al. 2003. “Flying Squirrel-Associated Typhus, United States.” Emerging Infectious Diseases 9:1341–1343.https://doi.org/10.3201/eid0910.030278
Tamura, A., N. Ohashi, H. Urakami, and S. Miyamura. 1995. “Classification of Rickettsia tsutsugamushi in a New Genus, Orientia gen. nov., as Orientia tsutsugamushi comb. nov.” International Journal of Systematic Bacteriology 45:589–591. https://doi.org/10.1099/00207713-45-3-589
Thorner, A. R., D. H. Walker, and W. A. Petri. 1998. “Rocky Mountain Spotted Fever.” Clinical Infectious Diseases 27:1353–1360. https://doi.org/10.1086/515037
Walker, D. H., and D. Raoult. 1995. “Rickettsia rickettsii and Other Spotted Fever Group Rickettsiae (Rocky Mountain Spotted Fever and Other Spotted Fevers).” In Mandell, Douglas, and Bennett's Principles and Oractices of Infectious Diseases, 4th edition, edited by G. L. Mendel, J. E. Bennett, and R. Dolin, 1721–1727. Philadelphia: Churchill Livingstone.
Wells, G. M., T. E. Woodward, P. Fiset, and R. B. Hornick. 1978. “Rocky Mountain Spotted Fever Caused by Blood Transfusion.” Journal of the American Medical Association 239:2763–2765. https://doi.org/10.1001/jama.239.26.2763