Credit: Jan Kaliciak/iStock/Thinkstock, © Jan Kaliciak
Why do we need phosphorus?
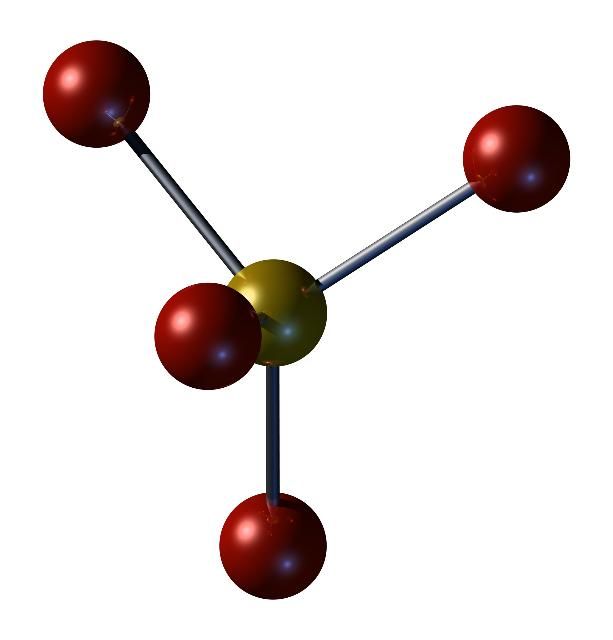
Phosphorus is a mineral found in every cell of the body, usually in the form of phosphate. It is the second most abundant mineral in the body after calcium. About 85% of phosphorus is stored in the bones and teeth. It is important for forming bones and teeth, as well as repairing bones. Phosphorus also helps:
- promote normal muscle and nerve function
- regulate heartbeat
- support growth and repair of cells and tissues
- store and use energy from food
- maintain normal kidney function
How much phosphorus do we need?
Recommended Dietary Allowances (RDA) for phosphorus intakes are listed in Table 1. Because high intakes of phosphorus pose health risks, Tolerable Upper Levels known as ULs have also been set to prevent overconsumption. Average daily intakes of phosphorus should not exceed the UL.
What is the availability of phosphorus in our diet?
Phosphorus is abundant in our diet. The three main sources of dietary phosphorus are food and beverages, food additives, and supplements. The main natural food sources are protein-rich foods such as meat, poultry, dairy products, eggs, legumes, and nuts. These foods provide about half of our dietary phosphorus (Calvo and Uribarri 2013a). Manufacturers add phosphorus to many processed foods to modify texture, taste, and color. Phosphorus added during food processing contributes an average of 500 mg per day (Calvo and Uribarri 2013a).
Because phosphorus is readily available in the diet, most people do not require phosphorus supplements. However, many supplements and medications contain phosphorus. For example, multivitamins and minerals contain, on average, more than 100 mg per tablet or capsule (Calvo and Uribarri 2013a). Many over-the-counter and prescription medications also contain phosphate salts as inactive ingredients (Calvo and Uribarri 2013a).
What happens if we do not get enough phosphorus?
Phosphorus is plentiful in the typical American diet, and so deficiency is rare. However, certain health conditions, such as starvation, alcoholism, and diabetic ketoacidosis, can cause low phosphorus levels. Also, certain medications, such as some antacids and diuretics, can cause phosphorus levels to decline (IOM 1997). The following are possible signs of low phosphorus in adults:
- poor appetite
- muscle weakness
- poor coordination
- bone pain
- fragile bones
The following are possible signs of low phosphorus in children:
- decline in growth
- poor bone and tooth development
*Note: These may be signs of other disease conditions
What happens if we get too much phosphorus?
Excessive intake of phosphorus is much more common than inadequate intake. Too much in the diet may lead to adverse effects on bone, kidney, and heart health (Calvo and Uribarri 2013b). Higher blood levels of phosphorus are usually the result of consuming large amounts of dietary phosphorus with insufficient dietary calcium. Kidney disease can also lead to an excess of phosphorus. If you have chronic kidney disease, you may need to limit your intake of phosphorus (CDC 2012). As kidney function decreases, extra phosphorus builds up in the blood. When there is too much phosphorus in the blood (hyperphosphatemia), calcium is lost from bones and deposited in tissues. This can lead to weak bones and cardiovascular disease. Persons with chronic kidney disease should consult their health care provider for specific dietary recommendations.
In healthy individuals, mildly elevated blood levels of phosphorus are thought to increase risk for bone and heart disease (Calvo and Uribarri 2013b). For most persons, reducing excess dietary phosphorus can be achieved by reducing consumption of processed foods that contain added phosphorus. For example, pancakes from a mix, frozen waffles, bacon, processed cheese, deli meats, and poultry, convenience dinner entrées, canned soups, and most restaurant and fast foods may contain phosphorus additives. Additionally, cola beverages contain phosphoric acid, a form of phosphorus. The key to lowering dietary intake of added phosphorus is to prepare foods from scratch using fresh, unprocessed ingredients.
Unfortunately, the phosphorus content of food is not found on the Nutrition Facts panel, making it difficult to determine which foods are higher in phosphorus. However, the ingredient list on the food package is very useful when making healthful food choices. Read the ingredient list on the food package to determine if the food contains a phosphorus/phosphate additive (Table 2). Ingredients are listed from most abundant to least abundant and additives are noted toward the end of the list. Avoiding foods with phosphate additives can help to lower your intake of phosphorus.
Individuals with chronic kidney disease should seek professional dietary advice regarding their diet choices.
Where can I find more information?
Registered dietitians may be able to provide you with more information about choosing a healthy diet. Consult your pharmacist and physician with questions about medications and supplements.
The Family and Consumer Sciences (FCS) agent at your local UF/IFAS Extension office may have more information about food and nutrition and may have classes for you to attend.
References
Calvo, MS, and J. Uribarri. 2013. “Contributions to Total Phosphorus Intake: All Sources Considered.” Seminars in Dialysis, 26(1): 54–61. https://doi.org/10.1111/sdi.12042
Calvo, MS, and J. Uribarri. 2013. “Public Health Impact of Dietary Phosphorus Excess on Bone and Cardiovascular Health in The General Population.” American Journal of Clinical Nutrition, 98(1): 6–15. https://doi.org/10.3945/ajcn.112.053934
CDC (Centers for Disease Control and Prevention). 2023. “Chronic Kidney Disease Initiative”. Accessed May 7, 2024. https://www.cdc.gov/kidneydisease/index.html
IOM (Institute of Medicine). 1997. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Accessed May 7, 2024. https://pubmed.ncbi.nlm.nih.gov/23115811/