This document is part of a series which addresses end-of-life concerns, entitled The Art of Goodbye.
Most people would prefer to delay or completely avoid discussions about death. Even if people feel inclined to talk with loved ones and health care providers about end-of-life concerns, they are frequently at a loss for the best way to begin a discussion and are unsure of the topics they should cover. It is difficult to cover every consideration because the process of dying does not always follow a logical course. It is unique to the individual's circumstances. Nonetheless, conversations about end-of-life care and advance directives can help ensure that the person's wishes are honored. These measures also eliminate much of the difficult decision-making that loved ones typically face at the time of their loved ones' passing. Communicating effectively and gathering as much information ahead of time help the participants achieve many of the intended goals.

Credit: UF/IFAS
Identifying Barriers to Discussing the End of Life
Talking about dying is not easy (California Health Foundation, 2012; Institute of Medicine, 2015; Pew Research Center, 2013). Consider the following barriers:
-
People do not want to burden their family.
-
In a mobile society where it is common to live away from extended family, people may not have experienced someone's death and therefore do not know what to expect emotionally and socially.
-
People may not have lost someone close to them. They may be unfamiliar with the many decisions that need to be made and laws that must be followed.
-
Family relationships may be complicated, particularly in cases involving divorce and remarriage.
-
People do not know how to start the conversation.
-
They are afraid of the costs of an attorney and final arrangements.
-
People may feel that these decisions are out of their hands.
-
They trust that their adult children will make the right decisions for them.
-
These decisions are simply too painful, scary, or off-limits to discuss.
-
Individuals may be estranged from their family.
Sometimes family members assume:
-
No one will listen to me if I bring this up.
-
I am the only one who is concerned with this. I will not be able to get through to others, and it is going to be really awkward.
-
It is the wrong time to talk about death.
-
Things will never be the same once I bring this up.
-
In this family, we do not discuss emotional issues that may create conflict.
-
There are too many other issues to deal with in life. This is just not important right now.
This issue may be difficult to discuss with health care providers as well (Institute of Medicine, 2015).
-
Health care providers may pass off the conversation to someone else.
-
Communication suffers when health care providers are hurried or dealing with a crisis.
-
Systems are not set up for advance care planning and physician training.
These discomforts, fears, and barriers stand in the way of opportunities for in-depth, face-to-face conversations that open the door to loving care and comfort at the end of life. When we do not have these important conversations outside of an illness or crisis, others are left to speculate about our values, fears, and goals. Are any of these factors keeping you from talking about your wishes with someone who can make decisions for you?
The Process of End-of-Life Communication
Communication about end-of-life concerns is a process. It is a series of recurring conversations about preferences and wishes with a loved one and a health care provider. Some experts recommend beginning these conversations as a young adult and continuing the dialogue for many years (Institute of Medicine, 2015). Other experts suggest starting these conversations during periods of mental, physical, and emotional wellness rather than periods of major illness. However, not everyone wants to talk about end-of-life issues in advance (Keating et. al, 2010).

Credit: UF/IFAS
Checklists and guides are helpful tools to have when considering medical care decisions. However, these documents only have real meaning when someone understands what the person truly wants. Forms cannot account for unanticipated events, such as a sudden accident, or anticipate all possible scenarios and decisions that must be made. In short, dying is frequently unpredictable (Bauchner & Fontanarosa, 2016).

Credit: UF/IFAS
This is not to say that such conversations will always go smoothly, or that family tensions will magically disappear. Sometimes, unresolved issues and conflicts as well as strained family relationships interfere. Occasionally, certain issues are never resolved, and loved ones are left with unanswered questions.
The important point is to have these conversations before there is a crisis. This way, family and health care providers know which medical interventions the individual wants based on values, clearly defined goals, and treatment preferences (Institute of Medicine, 2014). The key is to work through the discomfort and have a talk while you are healthy and able to make decisions. Conflict can even be positive if it helps you and your loved ones learn and understand more about each other.

Credit: UF/IFAS
Communicating with Loved Ones
It may not be easy to open up a conversation as a caregiver, family member, or older adult. An excellent resource is The Conversation Starter Kit, produced by The Conversation Project (http://theconversationproject.org/starter-kit/go/). This simple and clearly written guide walks people through the steps of what may be considered "The Most Important Conversation You Will Ever Have" (CNN, 2012).
These questions are intended to prepare you for the conversation.
-
With whom do you want to speak? Whom do you trust to speak for you?
-
When would be a good time to talk?
-
Where would you feel comfortable talking?
-
What do you want to say?
To begin, find a natural opening in a conversation or make a simple and heartfelt statement to engage the trusted individual. The Conversation Project recommends these types of statements:
-
"I need your help with something."
-
"I was thinking about [someone in the family] and it made me realize..."
-
"I need to talk about the future. Will you help me?"
-
"I just filled in a booklet answering some questions about what I want at the end of life. Would you look at this with me? I would like to talk about it and want you to see my answers. And I'm wondering what your answers would be." (The Conversation Project, 2014)
The Conversation Project also provides several suggestions to keep the conversation flowing.
-
Be patient so people have time to think and speak.
-
Let the conversation progress naturally without attempting to steer it in a certain direction or hurry things along. Let the person talk in his or her own way.
-
Remember to listen. This means giving your full attention to the other speakers, hearing them out, and expressing your understanding of their thoughts and feelings.
-
Do not judge. People have different ideas about what a "good death" means to them.
-
Ask open-ended questions that encourage discussion, such as "What do you think?" and "How do you feel?"
-
Do not keep going if people are exhausted and uncomfortable. This is only one conversation—you do not have to cover everything at once.
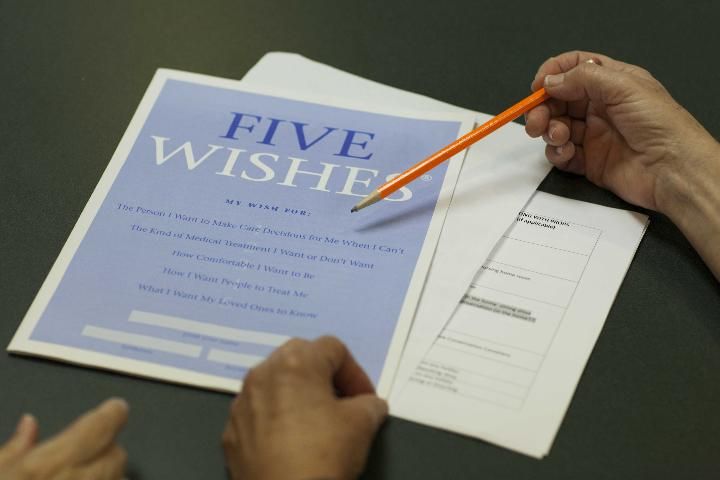
Another excellent resource on communication about medical treatment is Five Wishes®, an advance directive that helps people identify and discuss their wishes for medical interventions. Five Wishes® frames the discussion around comfort, dignity, and family involvement (Institute of Medicine, 2015). Written in nontechnical language, Five Wishes® helps begin the conversation, guides it along, and encourages completion of advance directives (Durbin, 2007). It addresses the following:
-
The person I want to make care decisions for me when I cannot
-
The kind of medical treatment I want or do not want
-
How comfortable I want to be
-
How I want people to treat me
-
What I want my loved ones to know (Aging with Dignity, 2016)
Credit: UF/IFAS
A good death is good care at the end of life.
Communicating with Health Care Providers
Communicating with health care providers as well as loved ones is a process. Studies find that the vast majority of adults want doctors to discuss end-of-life care issues with them. However, fewer than 20% report engaging in that conversation (California Health Foundation, 2012; Kaiser Family Foundation, 2015). Other studies have found that, when faced with a terminal illness, few patients want to talk about the prognosis early (cited in Keating et al., 2010).
One study reported that many doctors delay talking about the end of life. For example, a study of 4,000 cancer doctors found that, when a hypothetical patient has six months to live, most physicians talk about the current prognosis. Approximately 25% talk about hospice care or preferred site of death, while 44% discuss preferences for resuscitation. Many would only talk about these issues if the patient or family specifically asked about them (Keating et al., 2010).
On one hand, physicians may not be trained to have these conversations (American Heart Association, 2014; Dunlay et al., 2015; Sullivan, Lakoma, & Block, 2003). A study of 94 physicians, nurse practitioners, and physician assistants found that 30% have little confidence in talking about or providing end-of-life care. 52% said they are hesitant to mention end-of-life care.
However, only a small minority feels uncomfortable (11%) or views lack of time as an obstacle (9%) (American Heart Association, 2014). Physicians may have many other reasons for not discussing a terminal prognosis or the end of life.
-
Health care providers may fear the patient will lose hope. However, studies find that these discussions may actually help ease the fears of the patient as well as the family (American Heart Association, 2014; Keating et al., 2010).
-
Providers may feel they have made inaccurate predictions or failed to cure the patient (Keating et al., 2010).
-
They may be unaware that the patient has advance directives (Kass-Barelmes, 2003).
-
They may also recognize that some patients do not want to discuss end-of-life matters early or, in certain cases, at all (Keating et al., 2010).
Conclusion
The process of discussing end-of-life issues and writing advance directives involves the individual, loved ones, and health care providers. Communication with health care providers is essential to ensure that everyone is on the same page and that the individual's preferences will be made a priority. For more information on these topics, see EDIS publication FY1467, The Art of Goodbye: Exploring Health Concerns (https://edis.ifas.ufl.edu/fy1467).
Additional Resources
StoryCorps: A free app from https://storycorps.me/ that allows family members to capture the legacy of loved ones to share with future generations. The app provides questions about family heritage or life in general and stores voice recordings of the interviews.
To Our Children's Children, Preserving Family Histories for Generations to Come by Bob Greene and D. G. Fulford: This book provides an array of questions you would never think to ask. Topics range from family history, childhood, adulthood, parenthood, home, habits, and grandparenthood to hobbies and more. These conversation starters are meant to help people capture personal histories as a gift for their descendants through tape recording, writing, or typing.
To Our Children's Children, Journal of Family Memories by Bob Greene and D. G. Fulford: This book provides space to write down memories using over 1,000 family-related questions and prompts. It is one way to create a beautiful keepsake that will be enjoyed for generations to come.
A Mother's Legacy: Your Life Story in Your Own Words by Thomas Nelson: This journal helps capture family history, traditions, and other personal information about loved ones. It is set up in a 12-month format. Each month offers questions and space to record answers.
The Book of Myself: A Do-It-Yourself Autobiography in 201 Questions by Carl and David Marshall: Divided into early, middle, and later years, the book/journal offers questions and space to record memories about family, friends, education, work, and other topics. This is one way to reflect on a life and share its memories with future generations.
References
Aging with Dignity. (2016). Five Wishes® Online. Accessed on October 24, 2016. https://agingwithdignity.org/five-wishes/five-wishes-online
American Heart Association. (2014). Doctors reluctant to discuss end-of-life care with heart failure patients: American Heart Association meeting report, Abstract 352. AHA/ASA Newsroom, June 4, 2014. Accessed on January 26, 2015. http://newsroom.heart.org/news/doctors-reluctant-to-discuss-end-of-life-care-with-heart-failure-patients
Benson, W. F., & Aldrich, N. (2012). Advance care planning: Ensuring your wishes are known and honored if you are unable to speak for yourself. Centers for Disease Control and Prevention. Accessed on July 29, 2016. http://www.cdc.gov/aging/pdf/advanced-care-planning-critical-issue-brief.pdf
Bravo, G., Arcand, M., Blanchette, D., Boire-Lavigne, A. M., Dubois, M. F., Guay, M....Bellemar, S. (2012). Promoting advance planning for health care and research among older adults: A randomized controlled trial. BMC Medical Ethics. DOI: 10.1186/1472-6939-13-1
California Health Care Foundation (CHCF). (2012). Poll finds wide gap between the care patients want and receive at the end of life. Accessed on Feburary 11, 2015. http://www.chcf.org/media/press-releases/2012/end-of-life-care
CNN. (2012). The most important conversation you'll ever have. Accessed on October 28, 2015. http://www.cnn.com/2012/09/27/living/oprah-important-conversation/index.html
The Conversation Project. (2014). Your conversation starter kit. Accessed on August 25, 2016. http://theconversationproject.org/starter-kit/go/
Dunlay, S. M., Foxen, J. L., Cole, T., Feely, M. A., Loth, A. R., Strand, J. J.... Redfield, M. M. (2015). A survey of clinician attitudes and self-reported practices regarding end-of-life care in heart failure. Palliative Medicine, 29(3), 260–267. DOI: 10.1177/0269216314556565
Durbin, C. R. (2007). Healthcare decision-making in community-dwelling adults (Dissertation). University of Missouri-St. Louis, St. Louis, MO.
Institute of Medicine (IOM). (2015). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academy of Sciences. Accessed on August 25, 2016. http://www.ncbi.nlm.nih.gov/books/NBK285677/
Kaiser Family Foundation. (2015). 10 FAQs: Medicare's role in end-of-life care. Accessed on October 24, 2016. http://kff.org/medicare/fact-sheet/10-faqs-medicares-role-in-end-of-life-care/
Keating, N. L., Landrum, M. B., Rogers, S. O., Baum, S. K., Virnig, B. A., Huskamp, H. A....Kahn, K. L. (2010). Physician factors associated with discussions about end-of-life care. Cancer, 116(4), 998–1006. DOI:10.1002/cncr.24761
Pew Research Center (2013). Views on end-of-life medical treatments. Accessed on December 20, 2014. http://www.pewforum.org/2013/11/21/views-on-end-of-life-medical-treatments/
Stum, M. S. (2012). Critical conversations about inheritance: Can we talk? University of Minnesota Extension. Accessed on July 29, 2016. http://www.extension.umn.edu/family/personal-finance/who-gets-grandmas-yellow-pie-plate/free-articles/critical-conversations/
Sullivan, A. M., Lakota, M. D., & Block, S. D. (2003). The status of medical education in end-of-life care: A national report. Journal of General Internal Medicine, 18(9), 685–695. DOI: 10.1046/j.1525-1497.2003.21215.x